The idea that pork consumption may cause cirrhosis has been around for a while. A fairly widely cited 1985 study by Nanji and French (
) provides one of the strongest indictments of pork: “In countries with low alcohol consumption, no correlation was obtained between alcohol consumption and cirrhosis. However, a significant correlation was obtained between cirrhosis and pork.”
Recently Paul Jaminet wrote a blog post on the possible link between pork consumption and cirrhosis (
). Paul should be commended for bringing this topic to the fore, as the implications are far-reaching and very serious. One of the key studies mentioned in Paul’s post is a 2009 article by Bridges (
), from which the graphs below were taken.
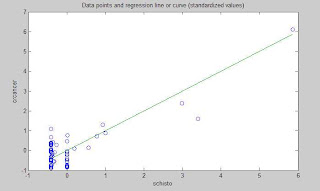
The graphs above show a correlation between cirrhosis and alcohol consumption of 0.71, and a correlation between cirrhosis and pork consumption of 0.83. That is, the correlation between cirrhosis and pork consumption is the stronger of the two! Combining this with the Nanji and French study, we have evidence that: (a) in countries with low alcohol consumption we can find a significant correlation between cirrhosis and pork consumption; and (b) in countries where both alcohol and pork are consumed, pork consumption has the strongest correlation with cirrhosis.
Do we need anything else to ban pork from our diets? Yes, we do, as there is more to this story.
Clearly alcohol and pork consumption are correlated as well, as we can see from the graphs above. That is, countries where alcohol is consumed more heavily also tend to have higher levels of pork consumption. If alcohol and pork consumption are correlated, then a multivariate analysis of their effects should be conducted, as one of the hypothesized effects (of alcohol or pork) on cirrhosis may even disappear after controlling for the other effect.
I created a dataset, as best as I could, based on the graphs from the Bridges article. (I could not get the data online.) I then entered it into WarpPLS (
). I wanted to run a moderating effect analysis, which is a form of nonlinear multivariate analysis. This is important, because the association between alcohol consumption and disease in general is well known to be nonlinear.
In fact, the relationship between alcohol consumption and disease is often used as a classic example of hormesis (
), and its characteristic J-curve shape. Since correlation is a measure of linear association, the lower correlation between alcohol consumption and cirrhosis, when compared with pork consumption, may be just a “mirage of linearity”. In multivariate analyses, this mirage of linearity may lead to what are known as type I and II errors, at the same time (
).
I should note that the Bridges study did something akin to a moderating effect analysis; through an analysis of the interaction between alcohol and pork consumption. However, in that analysis the values of the variables that were multiplied to create a “dummy” interaction variable were on their original scales, which can be a major source of bias. A more advisable way to conduct an interaction effect analysis is to first make the variables dimensionless, by standardizing them, and then creating a dummy interaction variable as a product of the two variables. That is what WarpPLS does for moderating effects’ estimation.
One more detour, leading to an important implication, and then we will get to the results. In a 1988 article, Jeanneret and colleagues show evidence of a strong and possibly causal association between alcohol consumption and protein-rich diets (
). One possible implication of this is that in countries where pork is a dietary staple, like Denmark and Germany, alcohol consumption should be strongly and causally associated with pork consumption. (I guess Anthony Bordain would agree with this eh?)
Below are the results of a multivariate analysis on a model that incorporates the above implication, by including a link between alcohol and pork consumption. The model also explores the role of pork consumption as a moderator of the relationship between alcohol and cirrhosis, as well as the direct effect of pork consumption on cirrhosis. Finally, the total effects of alcohol and pork consumption on cirrhosis are also investigated; they are shown on the left.
The total effects are both statistically significant, with
the total effect of alcohol consumption being 94 percent stronger than the total effect of pork consumption on cirrhosis. Looking at the model, alcohol consumption is strongly associated with pork consumption (which is consistent with Jeanneret and colleagues’s study). Alcohol consumption is also strongly associated with cirrhosis, through a direct effect; much more so than pork. Finally, pork consumption seems to strengthen the relationship between alcohol consumption and cirrhosis (the moderating effect).
As we can see
the relationship between pork consumption and cirrhosis is still there, in moderating and direct effects, even though it seems to be a lot weaker than that between alcohol consumption and cirrhosis.
Why does pork seem to influence cirrhosis at all in this dataset?Well,
there is another factor that is strongly associated with cirrhosis, and that is obesity (
). In fact, obesity is associated with just about any major disease, including various types of cancer (
).
And in countries where pork is a dietary staple, isn’t it reasonable to assume that pork consumption will play a role in obesity? Often folks who consume a lot of addictive industrial foods (e.g., bread, candy, regular sodas) also eat plenty of foods with saturated fat; and the latter end up showing up in disease statistics, misleadingly supporting the lipid hypothesis. The phenomenon involving pork and cirrhosis may well be similar.
But you may find the above results and argument not convincing enough. Maybe you want to see some evidence that pork is actually good for one’s health. The results above suggest that it may not be bad at all, if you buy into the obesity angle, but not that it can be good.
So I downloaded the most recent data from Nationmaster.com (
) on the following variables: pork consumption, alcohol consumption, and life expectancy. The list of countries was a bit larger than and different from that in the Bridges study; the following countries were included: Australia, Brazil, Canada, China, Denmark, France, Germany, Hong Kong, Hungary, Japan, Mexico, Poland, Russia, Singapore, Spain, Sweden, United Kingdom, and United States. Below are the results of a simple multivariate analysis with WarpPLS.

As with the Bridges dataset, there is a strong multivariate association between alcohol and pork consumption (0.43). The multivariate association between alcohol consumption and life expectancy is negative (-0.14). The multivariate association between pork consumption and life expectancy is positive (0.36). Neither association is statistically significant, although the association involving pork consumption gets close to significance with a P=0.11 (a confidence level of 89 percent; calculated through jackknifing, a nonparametric technique). The graphs show the plots for the associations and the best-fitting lines; the blue dashed arrows indicate the multivariate associations to which the graphs refer. So, in this second dataset from Nationmaster.com,
the more pork is consumed in a country, the longer is the life expectancy in that country.
In other words, for each 1 standard deviation variation in pork consumption, there is a 0.36 standard deviation variation in life expectancy, after we control for alcohol consumption. The standard deviation for pork consumption is 36.281 lbs/person/year, or 45.087 g/person/day; for life expectancy, it is 4.677 years. Working the numbers a bit more, the results above suggest that
each extra gram of pork consumed per person per day is associated with approximately 13 additional days of overall life expectancy in a country! This is calculated as: 4.677/45.087*0.36*365 = 13.630.
Does this prove that eating pork will make you live longer? No single study will “prove” something like that. Pork consumption is also likely a marker for wealth in a country; and wealth is strongly and positively associated with life expectancy at the country level. Moreover, when you aggregate dietary and disease incidence data by country, often the statistical effects are caused by those people in the dietary extremes (e.g., alcohol abuse, not moderate consumption). Finally, if people avoid death from certain diseases, they will die in higher quantities from other diseases, which may bias statistical results toward what may look like a higher incidence of those other diseases.
What the results summarized in this post do suggest is that
pork consumption may not be a problem at all, unless you become obese from eating it. How do you get obese from eating pork? Eating it together with industrial foods that are addictive would probably help.