Michael Holick, MD, PhD, of Boston University Medical Center says he’s “just one of the many scientists” exploring vitamin D, but he easily can be considered the world’s foremost authority on the sunshine vitamin.
In the 1970s, it was Dr. Holick who first isolated the major circulating form of vitamin D in plasma, 25-hydroxyvitamin D, as well as the active form produced by the kidneys.
He was also one of the first scientists to warn the medical community about the potential implications of widespread vitamin D insufficiency. When asked about the prevalence of low vitamin D status, he answers that it’s the “most common medical condition in the world, believe it or not.”
Dr. Holick has championed the cause of bringing vitamin D into the limelight for decades, writing numerous scientific papers as well as two popular books on the subject of vitamin D and health.
Getting D Facts from Dr. Holick
While seeking the latest findings from vitamin D research, I caught up with Dr. Holick and sought out his advice on sun exposure, vitamin D supplementation and vitamin D’s potential ties to weight management, insulin resistance and heart health.*
Q: Dr. Holick, thank you for taking the time to update us on vitamin D research. Elvis Presley once said, “Truth is like the sun. You can shut it out for a time, but it ain’t going away.” Don’t you think this quote represents the vitamin D story?
A: Amen. Elvis was right on target. Our sun has been demonized for 40 years unchallenged. It’s quite remarkable that it’s part of the psyche of the world. But it’s caused a major problem, which is worldwide vitamin D deficiency [or insufficiency] and markedly increased risk of chronic disease for children and adults.
You can instantly make vitamin D, but if you’re avoiding the sun as most people do it puts you at high-risk of deficiency. Why is that? It’s been demonized for so long because the dermatologists have come out with the big “C” word [melanoma skin cancer from sun exposure]. And there’s no question that skin cancer is on the rise. The major reason is because back in the ’60s people used to put baby oil on and bake in the sun. Right? Now, all of the sudden, that’s starting to haunt them later in life. It increased their risk of non-melanoma skin cancer.
But often what people don’t realize is that melanoma, the most deadly cancer—which is also what they lump together with skin cancer from the sun—most melanomas occur on the least sun-exposed areas. Occupational sun exposure decreases your risk of developing melanoma. There was a study done in a group in Texas that if you had the most sun exposure as a child and young adult and you did get melanoma, then you were more likely to survive it.
Q: Would you comment on vitamin D being a hormone, and the oldest hormone?
A: Well, the reason why we say that [it's the oldest hormone] is because I asked the question several years ago. If you take phytoplankton—there’s a phytoplankton species called Emiliani huxleii has been identified as one of the oldest phytoplankton species that has been unchanged for 750 million years. When we looked at that organism, it made a huge amount of vitamin D when it was exposed to sunlight.
It’s a hormone you make in your skin, then it’s inactive. It has to go to your liver to get hydroxylated to 25-hydroxyvitamin D, which is the major circulating form, the form you should ask your doctor to test for vitamin D status. Then it goes to your kidneys where it’s activated to 1,25-dihydroxyvitamin D, then it goes to your bone and intestines and kidneys.
Q: As a hormone, we also know now that it has a greater role on the body besides speeding up absorption of calcium for bone health. There is a link to cardiovascular health, right? What’s the state of the science?
A: As for the heart, we know that vascular smooth muscle cells have vitamin D receptors and we know that vitamin D seems to play a role in regulating blood pressure, regulating heart muscle cells in their growing activity, regulates to some degree the strength of the heart in terms of its pumping ability. That’s why it’s not at all surprising that just two years ago out of the Framingham heart study it shows that if you are vitamin D deficient you [are not providing optimal support for cardiovascular health].
Q: How does vitamin D’s relationship to heart health affect you if you are overweight?
A: This issue for obese people is particularly important because vitamin D is fat-soluble and is incorporated in your body fat. We showed many years ago that if you take an obese person and give him an oral dose of vitamin D or put him in a [UVB] tanning bed, it only raises his blood level to less than 50 percent than what a normal-weighted individual does and we’re talking about a BMI [Body Mass Index] of greater than 30. He needs two to three times more [of vitamin D than a person of normal BMI].
We know that obese people have more aches in their muscles, which is definitely due to vitamin D deficiency. They have muscle weakness. They’re fatigued. They just don’t want to go. It’s in part due to the deficiency. We also know that fat cells have a vitamin D receptor. There’s some evidence—we’re doing some research right now—that suggests that maybe vitamin D helps keep fat cells in check.
Q: Really? By what mechanism is it that you think vitamin D could help keep fat cells in check?
A: It may regulate fat cell maturation. It may regulate fat cell fat accumulation. That’s brand new stuff that we’re taking a look at that we’ve not yet published on. We’re just beginning to look at it.
Q: Is there any relationship established between low vitamin D status and insulin sensitivity?
A: We think so. We know that from NHANES (National Health and Nutritional Examination Survey) that [there may be a relationship associated with insulin sensitivity].
Q: We’ve heard a lot about a new established relationship between vitamin D and the immune system. Would you comment on the mechanism by which vitamin D is involved?
A: Well we know is that your immune system is regulated by vitamin D. We know that the cell macrophages definitely gobble up infectious agents because of vitamin D, macrophages activate vitamin D locally, and it stimulates production of a defensive protein that kills infectious agents. A study was done to show that if you raise your blood level, that you have more activity of your macrophages in killing infective agents. If there’s anything out there that helps to support the immune system, it’s probably vitamin D.
Q: Do you agree that everyone should be checked for vitamin D status?
A: Well, that’s the problem. It’s not an unreasonable thing to do, but I can already tell you they’re deficient. We know almost everyone’s deficient. If a normal adult isn’t taking at least 1,500 to 2,000 IU from supplement and diet—and you can’t really get it from your diet—then we know you’re vitamin D deficient. And so, to try to screen everybody, all the obese people in the United States is such a huge cost burden.
In fact, Medicare is looking at this right now and wanting to control the doctors’ use of that assay. They do not want to use it as a screening tool. I don’t disagree with that. Because we know that you can very effectively correct vitamin D deficiency, treat it, and prevent it from occurring again, if you give the person enough vitamin D. So only if they have fat malabsorption syndrome, or has had gastric bypass surgery, or cystic fibrosis, IBD, or celiac sprue—all of those individuals should be tested because you can’t predict whether or not they’re going to be able to absorb the vitamin D that you give them as a supplement.
Q: What about older people? Does the requirement for vitamin D supplementation increase with older age because of declined absorption?
A: No it does not. That’s what everybody says. [Note: Elderly can absorb vitamin D as easily as younger people.] What does change with age is the ability to make it in your skin. We showed many years ago that if you compare a 70-year-old to a 20-year-old, the 70-year-old will have about a 70 percent reduced ability to produce vitamin D. But we also went on to show that you can take an older person and still have them exposed to sunlight or simulated sunlight and they make a lot of vitamin D. Your body has a huge capacity to make vitamin D. We showed that healthy adults in bathing suits getting a minimal erythermal dose get an equivalent to ingesting 20,000 IU of vitamin D.
Now you begin to understand why the 100 IU in a glass of milk or orange juice or the 400 IU in a multivitamin is probably one tenth of what we really need to satisfy our body’s requirements for heart health or for reducing risk diseases.
Q: Do you agree as other scientists have suggested that the average person should be getting at least 20 minutes of sunshine per day for adequate vitamin D intake along with supplementation?
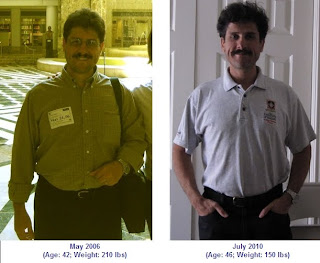
Dr. Holick has been researching vitamin D since the 1970s.
A: I don’t know about 20 minutes a day because it depends upon time of day, season of the year, latitude, and your degree of skin pigmentation. What I tell people is, if you know that you’re going to be out in June at noon-time for 30 minutes, in Arizona, and you’re going to get a light sunburn to your skin, to go out 50 percent of that time.
Always protect your face, it’s the most sun exposed, the most sun damaged. But you can certainly expose your arms and legs and not worry about it, in my opinion. Abdomen, back, not a problem. The more skin you expose, the more [vitamin D] that you make.
Q: Do you expect the Institute of Medicine’s recommendations for Adequate Intake of vitamin D to change in the United States anytime soon to reflect findings of new research?
A: Yes, there will definitely be new Adequate Intakes. What you really care about though is not the AI recommendation, what you care about is the Upper Limit—that’s what prevents manufacturers from putting vitamin D into foods. The amounts that you can put in and the amounts that supplements can contain.
The safe upper limit right now is considered to be 2,000 IU for adults. The major manufacturers like Coca Cola or who make Minute Maid orange juice for example put only 100 IU in a glass, because if they put in any more then they start adding that up, drinking milk and taking a multivitamin, you’re over the 2,000 IU limit.
Then if you get some toxicity like a kidney stone, it doesn’t matter that it’s not due to the vitamin D, the lawyers will say that it is if you put more than you should’ve put in. So they need to increase it like to 10,000 IU in which case, then we can really have an impact on the entire U.S. population and the world’s population because they could now put more vitamin D in the food.
Q: Dr. Holick, this has been very interesting and I’m sure it will be interesting to our readers. Thank you for your time. Also, congrats on the new book. We’ll be ordering a couple of copies for our library.
A: Wonderful. Feel free to stay in touch