Filet mignon is one of the tenderest cuts of beef. It is also one of my favorites. Filet mignon comes from the tenderloin area (see this picture), which is not a weight-bearing area and thus is very tender. The bison cuts I get here in South Texas are close in terms of tenderness, but not as tender, probably because they are from the round area.
One steak of either filet mignon or bison will yield about 100 g of cooked meat, with 30 g of protein and 10 g of fat. About half of that fat will be saturated and half monounsaturated (as in olive oil). It will provide you with plenty of vitamins (particular B vitamins) and minerals. Good amounts of selenium, phosphorus, zinc and potassium.
On the photo below (click on it to enlarge), the bison steak is at the top. The other pieces are all filet mignon cuts. They are all medium-cooked. I cooked two plates of these, for 6 people. All ate to satisfaction, with a side salad. The leftovers are delicious for breakfast in small amounts.
For the filet mignon, I think you really have to go to a specialty meats store (butcher) and make sure that they cut the smaller tail end of the tenderloin muscle. You will be paying a lot for it, so it makes sense to be choosy. Experience butchers will cut it right in front of you and won’t mind your choosiness.
Below is a simple recipe; simple like most of the recipes on this blog. I like my meals quick and delicious.
- Prepare some dry seasoning powder by mixing sea salt, garlic power, chili powder, and a small amount of cayenne pepper.
- Season the steaks at least 2 hours prior to placing them on the grill.
- Grill with the lid on, checking the meat every 10 minutes or so. (I use charcoal, one layer only to avoid burning the surface of the meat.) Turn it frequently, always putting the lid back on.
- If you like it rare, 20 minutes (or a bit less) may be enough.
These are as tender as any piece of beef can possibly get. No need for any tenderizer juices during seasoning. If you are doing both filet mignon and bison together, either eat only bison or bison first. Because once you taste the filet mignon, the bison cut may taste a bit hard!
For me the filet mignon is a 10-dollar per pound treat for special occasions. The price of the bison cut is about the same, at least here in Laredo, Texas, where I get it shipped from Dakota via my local supermarket. You can also get it online.
By the way, some folks like to say that bison is the “salmon of the prairie”. This is in reference to bison’s omega-3 content. Well, here is the polyunsaturated fatty acid composition of 100 g of bison steak: 29 mg of omega-3, and 197 mg of omega-6. For salmon it is 1424 mg of omega-3, and 113 mg of omega-6.
Salmon of the prairie or not, I love it!
Thursday, April 29, 2010
Tuesday, April 27, 2010
Cordain vs Campbell
I recently read what is entitled the "Protein Debate" between Loren Cordain, a paleo diet proponent, and Colin Campbell, a plant-based diet proponent. Given that I'm simply a graduate student without any specific adherence to either diet philosophy, i found the debate to be fascinating. Both had strong points to defend their positioning. In short, this is how it goes:
- Loren Cordain argues that because nutritional science is a young, evolving science with little agreement as to what is correct in eating for the general population, they should have a "guiding paradigm" based on the diet of our hunter-gatherer ancestors. The paleolithic diet would be one that include high amounts of protein from lean meats and minimally processed foods of paleolithic resemblance.
- Colin Campbell argues that nutritional science is not young (it's older than many other sciences) and, that, although knowledge of ancestral diets may be helpful, "biological complexity" throws out its use as a reference standard (after all, high calorie intake from meat may have increased likelihood of reproduction, but not guarded against disease). The priority should be given to searching for dietary factors that cause "collective disease and health outcomes" to guide nutritional recommendations.
Labels:
nutr therap
Monday, April 26, 2010
Blood glucose control before age 55 may increase your chances of living beyond 90
I have recently read an interesting study by Yashin and colleagues (2009) at Duke University’s Center for Population Health and Aging. (The full reference to the article, and a link, are at the end of this post.) This study is a gem with some rough edges, and some interesting implications.
The study uses data from the Framingham Heart Study (FHS). The FHS, which started in the late 1940s, recruited 5209 healthy participants (2336 males and 2873 females), aged 28 to 62, in the town of Framingham, Massachusetts. At the time of Yashin and colleagues’ article publication, there were 993 surviving participants.
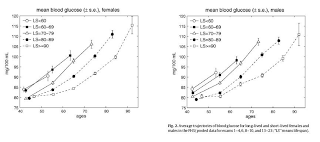
I rearranged figure 2 from the Yashin and colleagues article so that the two graphs (for females and males) appeared one beside the other. The result is shown below (click on it to enlarge); the caption at the bottom-right corner refers to both graphs. The figure shows the age-related trajectory of blood glucose levels, grouped by lifespan (LS), starting at age 40.
As you can see from the figure above, blood glucose levels increase with age, even for long-lived individuals (LS > 90). The increases follow a U-curve (a.k.a. J-curve) pattern; the beginning of the right side of a U curve, to be more precise. The main difference in the trajectories of the blood glucose levels is that as lifespan increases, so does the width of the U curve. In other words, in long-lived people, blood glucose increases slowly with age; particularly up to 55 years of age, when it starts increasing more rapidly.
Now, here is one of the rough edges of this study. The authors do not provide standard deviations. You can ignore the error bars around the points on the graph; they are not standard deviations. They are standard errors, which are much lower than the corresponding standard deviations. Standard errors are calculated by dividing the standard deviations by the square root of the sample sizes for each trajectory point (which the authors do not provide either), so they go up with age since progressively smaller numbers of individuals reach advanced ages.
So, no need to worry if your blood glucose levels are higher than those shown on the vertical axes of the graphs. (I will comment more on those numbers below.) Not everybody who lived beyond 90 had a blood glucose of around 80 mg/dl at age 40. I wouldn't be surprised if about 2/3 of the long-lived participants had blood glucose levels in the range of 65 to 95 at that age.
Here is another rough edge. It is pretty clear that the authors’ main independent variable (i.e., health predictor) in this study is average blood glucose, which they refer to simply as “blood glucose”. However, the measure of blood glucose in the FHS is a very rough estimation of average blood glucose, because they measured blood glucose levels at random times during the day. These measurements, when averaged, are closer to fasting blood glucose levels than to average blood glucose levels.
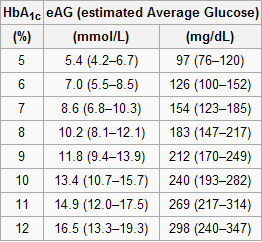
A more reliable measure of average blood glucose levels is that of glycated hemoglobin (HbA1c). Blood glucose glycates (i.e., sticks to, like most sugary substances) hemoglobin, a protein found in red blood cells. Since red blood cells are relatively long-lived, with a turnover of about 3 months, HbA1c (given in percentages) is a good indicator of average blood glucose levels (if you don’t suffer from anemia or a few other blood abnormalities). Based on HbA1c, one can then estimate his or her average blood glucose level for the previous 3 months before the test, using one of the following equations, depending on whether the measurement is in mg/dl or mmol/l.
Average blood glucose (mg/dl) = 28.7 × HbA1c − 46.7
Average blood glucose (mmol/l) = 1.59 × HbA1c − 2.59
The table below, from Wikipedia, shows average blood glucose levels corresponding to various HbA1c values. As you can see, they are generally higher than the corresponding fasting blood glucose levels would normally be (the latter is what the values on the vertical axes of the graphs above from Yashin and colleagues’ study roughly measure). This is to be expected, because blood glucose levels vary a lot during the day, and are often transitorily high in response to food intake and fluctuations in various hormones. Growth hormone, cortisol and noradrenaline are examples of hormones that increase blood glucose. Only one hormone effectively decreases blood glucose levels, insulin, by stimulating glucose uptake and storage as glycogen and fat.
Nevertheless, one can reasonably expect fasting blood glucose levels to have been highly correlated with average blood glucose levels in the sample. So, in my opinion, the graphs above showing age-related blood glucose trajectories are still valid, in terms of their overall shape, but the values on the vertical axes should have been measured differently, perhaps using the formulas above.
Ironically, those who achieve low average blood glucose levels (measured based on HbA1c) by adopting a low carbohydrate diet (one of the most effective ways) frequently have somewhat high fasting blood glucose levels because of physiological (or benign) insulin resistance. Their body is primed to burn fat for energy, not glucose. Thus when growth hormone levels spike in the morning, so do blood glucose levels, as muscle cells are in glucose rejection mode. This is a benign version of the dawn effect (a.k.a. dawn phenomenon), which happens with quite a few low carbohydrate dieters, particularly with those who are deep in ketosis at dawn.
Yashin and colleagues also modeled relative risk of death based on blood glucose levels, using a fairly sophisticated mathematical model that takes into consideration U-curve relationships. What they found is intuitively appealing, and is illustrated by the two graphs at the bottom of the figure below. The graphs show how the relative risks (e.g., 1.05, on the topmost dashed line on the both graphs) associated with various ranges of blood glucose levels vary with age, for both females and males.
What the graphs above are telling us is that once you reach old age, controlling for blood sugar levels is not as effective as doing it earlier, because you are more likely to die from what the authors refer to as “other causes”. For example, at the age of 90, having a blood glucose of 150 mg/dl (corrected for the measurement problem noted earlier, this would be perhaps 165 mg/dl, from HbA1c values) is likely to increase your risk of death by only 5 percent. The graphs account for the facts that: (a) blood glucose levels naturally increase with age, and (b) fewer people survive as age progresses. So having that level of blood glucose at age 60 would significantly increase relative risk of death at that age; this is not shown on the graph, but can be inferred.
Here is a final rough edge of this study. From what I could gather from the underlying equations, the relative risks shown above do not account for the effect of high blood glucose levels earlier in life on relative risk of death later in life. This is a problem, even though it does not completely invalidate the conclusion above. As noted by several people (including Gary Taubes in his book Good Calories, Bad Calories), many of the diseases associated with high blood sugar levels (e.g., cancer) often take as much as 20 years of high blood sugar levels to develop. So the relative risks shown above underestimate the effect of high blood glucose levels earlier in life.
Do the long-lived participants have some natural protection against accelerated increases in blood sugar levels, or was it their diet and lifestyle that protected them? This question cannot be answered based on the study.
Assuming that their diet and lifestyle protected them, it is reasonable to argue that: (a) if you start controlling your average blood sugar levels well before you reach the age of 55, you may significantly increase your chances of living beyond the age of 90; (b) it is likely that your blood glucose levels will go up with age, but if you can manage to slow down that progression, you will increase your chances of living a longer and healthier life; (c) you should focus your control on reliable measures of average blood glucose levels, such as HbA1c, not fasting blood glucose levels (postprandial glucose levels are also a good option, because they contribute a lot to HbA1c increases); and (d) it is never too late to start controlling your blood glucose levels, but the more you wait, the bigger is the risk.
References:
Taubes, G. (2007). Good calories, bad calories: Challenging the conventional wisdom on diet, weight control, and disease. New York, NY: Alfred A. Knopf.
Yashin, A.I., Ukraintseva, S.V., Arbeev, K.G., Akushevich, I., Arbeeva, L.S., & Kulminski, A.M. (2009). Maintaining physiological state for exceptional survival: What is the normal level of blood glucose and does it change with age? Mechanisms of Ageing and Development, 130(9), 611-618.
The study uses data from the Framingham Heart Study (FHS). The FHS, which started in the late 1940s, recruited 5209 healthy participants (2336 males and 2873 females), aged 28 to 62, in the town of Framingham, Massachusetts. At the time of Yashin and colleagues’ article publication, there were 993 surviving participants.
I rearranged figure 2 from the Yashin and colleagues article so that the two graphs (for females and males) appeared one beside the other. The result is shown below (click on it to enlarge); the caption at the bottom-right corner refers to both graphs. The figure shows the age-related trajectory of blood glucose levels, grouped by lifespan (LS), starting at age 40.
As you can see from the figure above, blood glucose levels increase with age, even for long-lived individuals (LS > 90). The increases follow a U-curve (a.k.a. J-curve) pattern; the beginning of the right side of a U curve, to be more precise. The main difference in the trajectories of the blood glucose levels is that as lifespan increases, so does the width of the U curve. In other words, in long-lived people, blood glucose increases slowly with age; particularly up to 55 years of age, when it starts increasing more rapidly.
Now, here is one of the rough edges of this study. The authors do not provide standard deviations. You can ignore the error bars around the points on the graph; they are not standard deviations. They are standard errors, which are much lower than the corresponding standard deviations. Standard errors are calculated by dividing the standard deviations by the square root of the sample sizes for each trajectory point (which the authors do not provide either), so they go up with age since progressively smaller numbers of individuals reach advanced ages.
So, no need to worry if your blood glucose levels are higher than those shown on the vertical axes of the graphs. (I will comment more on those numbers below.) Not everybody who lived beyond 90 had a blood glucose of around 80 mg/dl at age 40. I wouldn't be surprised if about 2/3 of the long-lived participants had blood glucose levels in the range of 65 to 95 at that age.
Here is another rough edge. It is pretty clear that the authors’ main independent variable (i.e., health predictor) in this study is average blood glucose, which they refer to simply as “blood glucose”. However, the measure of blood glucose in the FHS is a very rough estimation of average blood glucose, because they measured blood glucose levels at random times during the day. These measurements, when averaged, are closer to fasting blood glucose levels than to average blood glucose levels.
A more reliable measure of average blood glucose levels is that of glycated hemoglobin (HbA1c). Blood glucose glycates (i.e., sticks to, like most sugary substances) hemoglobin, a protein found in red blood cells. Since red blood cells are relatively long-lived, with a turnover of about 3 months, HbA1c (given in percentages) is a good indicator of average blood glucose levels (if you don’t suffer from anemia or a few other blood abnormalities). Based on HbA1c, one can then estimate his or her average blood glucose level for the previous 3 months before the test, using one of the following equations, depending on whether the measurement is in mg/dl or mmol/l.
Average blood glucose (mg/dl) = 28.7 × HbA1c − 46.7
Average blood glucose (mmol/l) = 1.59 × HbA1c − 2.59
The table below, from Wikipedia, shows average blood glucose levels corresponding to various HbA1c values. As you can see, they are generally higher than the corresponding fasting blood glucose levels would normally be (the latter is what the values on the vertical axes of the graphs above from Yashin and colleagues’ study roughly measure). This is to be expected, because blood glucose levels vary a lot during the day, and are often transitorily high in response to food intake and fluctuations in various hormones. Growth hormone, cortisol and noradrenaline are examples of hormones that increase blood glucose. Only one hormone effectively decreases blood glucose levels, insulin, by stimulating glucose uptake and storage as glycogen and fat.
Nevertheless, one can reasonably expect fasting blood glucose levels to have been highly correlated with average blood glucose levels in the sample. So, in my opinion, the graphs above showing age-related blood glucose trajectories are still valid, in terms of their overall shape, but the values on the vertical axes should have been measured differently, perhaps using the formulas above.
Ironically, those who achieve low average blood glucose levels (measured based on HbA1c) by adopting a low carbohydrate diet (one of the most effective ways) frequently have somewhat high fasting blood glucose levels because of physiological (or benign) insulin resistance. Their body is primed to burn fat for energy, not glucose. Thus when growth hormone levels spike in the morning, so do blood glucose levels, as muscle cells are in glucose rejection mode. This is a benign version of the dawn effect (a.k.a. dawn phenomenon), which happens with quite a few low carbohydrate dieters, particularly with those who are deep in ketosis at dawn.
Yashin and colleagues also modeled relative risk of death based on blood glucose levels, using a fairly sophisticated mathematical model that takes into consideration U-curve relationships. What they found is intuitively appealing, and is illustrated by the two graphs at the bottom of the figure below. The graphs show how the relative risks (e.g., 1.05, on the topmost dashed line on the both graphs) associated with various ranges of blood glucose levels vary with age, for both females and males.
What the graphs above are telling us is that once you reach old age, controlling for blood sugar levels is not as effective as doing it earlier, because you are more likely to die from what the authors refer to as “other causes”. For example, at the age of 90, having a blood glucose of 150 mg/dl (corrected for the measurement problem noted earlier, this would be perhaps 165 mg/dl, from HbA1c values) is likely to increase your risk of death by only 5 percent. The graphs account for the facts that: (a) blood glucose levels naturally increase with age, and (b) fewer people survive as age progresses. So having that level of blood glucose at age 60 would significantly increase relative risk of death at that age; this is not shown on the graph, but can be inferred.
Here is a final rough edge of this study. From what I could gather from the underlying equations, the relative risks shown above do not account for the effect of high blood glucose levels earlier in life on relative risk of death later in life. This is a problem, even though it does not completely invalidate the conclusion above. As noted by several people (including Gary Taubes in his book Good Calories, Bad Calories), many of the diseases associated with high blood sugar levels (e.g., cancer) often take as much as 20 years of high blood sugar levels to develop. So the relative risks shown above underestimate the effect of high blood glucose levels earlier in life.
Do the long-lived participants have some natural protection against accelerated increases in blood sugar levels, or was it their diet and lifestyle that protected them? This question cannot be answered based on the study.
Assuming that their diet and lifestyle protected them, it is reasonable to argue that: (a) if you start controlling your average blood sugar levels well before you reach the age of 55, you may significantly increase your chances of living beyond the age of 90; (b) it is likely that your blood glucose levels will go up with age, but if you can manage to slow down that progression, you will increase your chances of living a longer and healthier life; (c) you should focus your control on reliable measures of average blood glucose levels, such as HbA1c, not fasting blood glucose levels (postprandial glucose levels are also a good option, because they contribute a lot to HbA1c increases); and (d) it is never too late to start controlling your blood glucose levels, but the more you wait, the bigger is the risk.
References:
Taubes, G. (2007). Good calories, bad calories: Challenging the conventional wisdom on diet, weight control, and disease. New York, NY: Alfred A. Knopf.
Yashin, A.I., Ukraintseva, S.V., Arbeev, K.G., Akushevich, I., Arbeeva, L.S., & Kulminski, A.M. (2009). Maintaining physiological state for exceptional survival: What is the normal level of blood glucose and does it change with age? Mechanisms of Ageing and Development, 130(9), 611-618.
Friday, April 23, 2010
There are more geniuses among men than among women, and more idiots too
Deary and colleagues (2007) conducted an interesting study on differences in intelligence scores among men and women. In the context of this blog, this study highlights yet one more counterintuitive and intriguing aspect of Darwinian evolution, adding to points previously made in other posts (see here, and here). Evolution may look simple at first glance, but that is a bit of a mirage. In my opinion, to really understand it one has to understand the mathematics underlying it, a lot of which comes from the field of population genetics.
What makes the study by Deary and colleagues (2007) particularly interesting is that its participants were opposite-sex siblings. This helped control for the influence of environmental factors. The downside is that the effect sizes might have been decreased, because of the high gene correlation among siblings, so we could expect larger differences between unrelated groups of men women. The differences, as you will see, are not in overall scores, but in score dispersion.
Let us get straight to the point made by the study. On average, men and women seem to score equally well on intelligence tests. The main difference is that there is more variation in the scores achieved by men than by women, which leads to an interesting effect: there are more geniuses and more idiots among men than among women.
This does NOT mean that a man’s genius is of a higher order; just that there is a tendency for more men to be geniuses (and idiots) than women in any random population sample. The women who are geniuses can be super geniuses, like two-time Nobel Prize winner Marie Curie, the first PERSON to receive such an honor. Albert Einstein is said that have greatly admired her intelligence.
As an illustration of this score dispersion effect, Deary and colleagues (2007) note that: “… for example, in terms of indices of scientific achievement, men were awarded 545 out of the 557 Nobel prizes awarded for science.” On the “idiot” end of the scale: there are a lot more men than women in prison, and one common denominator of prison inmates is that they tend to score very low on intelligence tests. (This is not to say that all criminals have low intelligence; perhaps mostly the ones that get caught do.)
Having said that, it is important to acknowledge that there are multiple types of intelligence, and even multi-indicator intelligence coefficients are usually poor approximations of an overall measure of intelligence (if there is one). This does not invalidate the main point of this post, which is related to score variability.
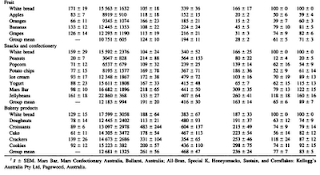
The table below (from: Deary and colleagues, 2007; click on it to enlarge; full reference at the end of this post) shows scores obtained by men and women (1,292 pairs of opposite-sex siblings) in various subtests of the Armed Services Vocational Aptitude Battery (ASVAB) test.
Note that nearly all of the differences between means (i.e., averages) are significant, but the direction of the differences (captured by the signs of the Cohen’s d coefficients, which are measures of effect size) varies a lot. That is, on several subtests (e.g., “Arithmetic”) men score higher, but in others (e.g., “Numerical operations”) women score higher. It all comes down to men and women scoring equally well overall.
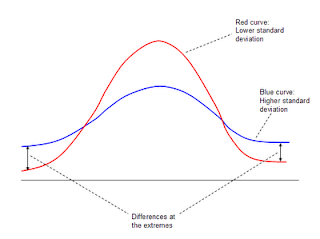
Now look at the columns showing the standard deviations (“SD”) for men and women. In all subtests but two (“Coding speed” and “Numerical operations”) the standard deviation is higher for men; in many cases significantly higher (e.g., 44 percent higher for “Mechanical comprehension”). The standard deviations are about the same for “Coding speed” and “Numerical operations”. What this means is that variability in scores is nearly always higher, often significantly higher, among men than among women. I prepared the schematic figure below to illustrate the effect that this has on the numbers of individuals at the extremes.
The figure above shows two (badly drawn) quasi-normal distributions of scores. (This post shows a better illustration of a normal distribution.) The red curve refers to a distribution with a lower standard deviation than the blue curve; the latter is flatter. Each point on a curve reflects the number of individuals obtaining a particular score, which would be indicated on the horizontal axis. The number of individuals with that score is on the vertical axis. As you can see, the numbers of individuals scoring very high and low (geniuses and idiots, if the scores reflected intelligence) are greater for the blue curve, which is the curve with the higher standard deviation (higher dispersion of scores). The farther one goes to the left or right (the extremes), the bigger this difference becomes.
What does this have to do with evolution?
Well, there are a few possibilities, two of which appear to be particularly compelling. Maybe this effect is due to a combination of these two.
One is that ancestral women, like women today, selected mating partners based on a wide range of traits. Ancestral men on the other hand, like modern men, focused on a much smaller set of traits (Buss, 1995). The end result is more variation in traits, generally speaking, among men than among women. This refers to traits in general, not only intelligence. For example, there seems to be more variation in height among men than among women.
The other possible explanation is that, in our ancestral past, staying out of the extremes of intelligence was associated with higher survival success in both sexes. It seems that the incidence of certain types of mental disease (e.g., schizophrenia) is quite high among geniuses. This leads to more deaths due to related issues – suicide, depression leading to the metabolic syndrome, etc. And this is today, where geniuses can find many opportunities to “shine” in our complex urban societies. In our ancestral past the cognitive demands would have been much lower, and so would the practical value of being a genius.
If staying out of the extremes has indeed enhanced survival success in our evolutionary past, then it is reasonable to expect more women to fit that pattern than men. As with almost any “thing” that enhances survival success, women (especially pre-menopausal) naturally have more of that “thing” than men (e.g., HDL cholesterol).
The reason is that women are more important for the survival of any population than men; today and 1 million years ago. A population of 99 women and 1 man can potentially generate 99 children every few years. Here inbreeding in subsequent generations will be a problem, but that is better than extinction. A population with 99 women and 99 men (or even 1,000 men) will not generate significantly more children.
Reference:
Buss, D.M. (2003). The evolution of desire: Strategies of human mating. New York, NY: Basic Books.
Deary, I.J., Irwing, P., Der, G., & Bates, T.C. (2007). Brother–sister differences in the g factor in intelligence: Analysis of full, opposite-sex siblings from the NLSY1979. Intelligence, 35(5), 451-456.
What makes the study by Deary and colleagues (2007) particularly interesting is that its participants were opposite-sex siblings. This helped control for the influence of environmental factors. The downside is that the effect sizes might have been decreased, because of the high gene correlation among siblings, so we could expect larger differences between unrelated groups of men women. The differences, as you will see, are not in overall scores, but in score dispersion.
Let us get straight to the point made by the study. On average, men and women seem to score equally well on intelligence tests. The main difference is that there is more variation in the scores achieved by men than by women, which leads to an interesting effect: there are more geniuses and more idiots among men than among women.
This does NOT mean that a man’s genius is of a higher order; just that there is a tendency for more men to be geniuses (and idiots) than women in any random population sample. The women who are geniuses can be super geniuses, like two-time Nobel Prize winner Marie Curie, the first PERSON to receive such an honor. Albert Einstein is said that have greatly admired her intelligence.
As an illustration of this score dispersion effect, Deary and colleagues (2007) note that: “… for example, in terms of indices of scientific achievement, men were awarded 545 out of the 557 Nobel prizes awarded for science.” On the “idiot” end of the scale: there are a lot more men than women in prison, and one common denominator of prison inmates is that they tend to score very low on intelligence tests. (This is not to say that all criminals have low intelligence; perhaps mostly the ones that get caught do.)
Having said that, it is important to acknowledge that there are multiple types of intelligence, and even multi-indicator intelligence coefficients are usually poor approximations of an overall measure of intelligence (if there is one). This does not invalidate the main point of this post, which is related to score variability.
The table below (from: Deary and colleagues, 2007; click on it to enlarge; full reference at the end of this post) shows scores obtained by men and women (1,292 pairs of opposite-sex siblings) in various subtests of the Armed Services Vocational Aptitude Battery (ASVAB) test.
Note that nearly all of the differences between means (i.e., averages) are significant, but the direction of the differences (captured by the signs of the Cohen’s d coefficients, which are measures of effect size) varies a lot. That is, on several subtests (e.g., “Arithmetic”) men score higher, but in others (e.g., “Numerical operations”) women score higher. It all comes down to men and women scoring equally well overall.
Now look at the columns showing the standard deviations (“SD”) for men and women. In all subtests but two (“Coding speed” and “Numerical operations”) the standard deviation is higher for men; in many cases significantly higher (e.g., 44 percent higher for “Mechanical comprehension”). The standard deviations are about the same for “Coding speed” and “Numerical operations”. What this means is that variability in scores is nearly always higher, often significantly higher, among men than among women. I prepared the schematic figure below to illustrate the effect that this has on the numbers of individuals at the extremes.
The figure above shows two (badly drawn) quasi-normal distributions of scores. (This post shows a better illustration of a normal distribution.) The red curve refers to a distribution with a lower standard deviation than the blue curve; the latter is flatter. Each point on a curve reflects the number of individuals obtaining a particular score, which would be indicated on the horizontal axis. The number of individuals with that score is on the vertical axis. As you can see, the numbers of individuals scoring very high and low (geniuses and idiots, if the scores reflected intelligence) are greater for the blue curve, which is the curve with the higher standard deviation (higher dispersion of scores). The farther one goes to the left or right (the extremes), the bigger this difference becomes.
What does this have to do with evolution?
Well, there are a few possibilities, two of which appear to be particularly compelling. Maybe this effect is due to a combination of these two.
One is that ancestral women, like women today, selected mating partners based on a wide range of traits. Ancestral men on the other hand, like modern men, focused on a much smaller set of traits (Buss, 1995). The end result is more variation in traits, generally speaking, among men than among women. This refers to traits in general, not only intelligence. For example, there seems to be more variation in height among men than among women.
The other possible explanation is that, in our ancestral past, staying out of the extremes of intelligence was associated with higher survival success in both sexes. It seems that the incidence of certain types of mental disease (e.g., schizophrenia) is quite high among geniuses. This leads to more deaths due to related issues – suicide, depression leading to the metabolic syndrome, etc. And this is today, where geniuses can find many opportunities to “shine” in our complex urban societies. In our ancestral past the cognitive demands would have been much lower, and so would the practical value of being a genius.
If staying out of the extremes has indeed enhanced survival success in our evolutionary past, then it is reasonable to expect more women to fit that pattern than men. As with almost any “thing” that enhances survival success, women (especially pre-menopausal) naturally have more of that “thing” than men (e.g., HDL cholesterol).
The reason is that women are more important for the survival of any population than men; today and 1 million years ago. A population of 99 women and 1 man can potentially generate 99 children every few years. Here inbreeding in subsequent generations will be a problem, but that is better than extinction. A population with 99 women and 99 men (or even 1,000 men) will not generate significantly more children.
Reference:
Buss, D.M. (2003). The evolution of desire: Strategies of human mating. New York, NY: Basic Books.
Deary, I.J., Irwing, P., Der, G., & Bates, T.C. (2007). Brother–sister differences in the g factor in intelligence: Analysis of full, opposite-sex siblings from the NLSY1979. Intelligence, 35(5), 451-456.
Labels:
evolution,
intelligence,
mating,
research,
survival
Wednesday, April 21, 2010
Interesting links
Below is a list of links to web sites that deal with health issues in general. I have moved them from the previous “favorite links” area to this post so that I could save some space on the main page of the blog. Some of them are excellent sources of research-based and reliable information. Others are somewhat light in content, but still interesting. I certainly do not agree with the ideas espoused by all of them.
Alan Aragon
http://www.alanaragon.com/
Animal Pharm
http://drbganimalpharm.blogspot.com/
Ancestralize Me!
http://www.ancestralizeme.com/
Anthony Colpo
http://anthonycolpo.com/
Arthur De Vany
http://www.arthurdevany.com/
At Darwin's Table
http://darwinstable.wordpress.com/
Athletics by Nature
http://gregcarver.com/blog
Barefoot Ted's Adventures
http://barefootted.com/
Beef and Whiskey
http://beefandwhiskey.com/
Big Muscles Fast
http://www.bigmusclesfast.com/
Blaine's Low Carb Kitchen
http://fittv.discovery.com/fansites/blaine/recipes/recipes.html
Blood Sugar 101
http://www.phlaunt.com/diabetes
Brad Pilon's Blog
http://bradpilon.com/
Canibais e Reis
http://www.canibaisereis.com/
Cholesterol and Health
http://www.cholesterol-and-health.com/
Colorado State University's Physiologic Effects of Insulin
http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/pancreas/insulin_phys.html
Conditioning Research
http://conditioningresearch.blogspot.com/
Cooling Inflammation
http://coolinginflammation.blogspot.com/
Cut the Carb
http://www.cutthecarb.com/
David Mendosa
http://www.healthcentral.com/diabetes/c/17
Diabetes Update
http://diabetesupdate.blogspot.com/
Diet Doctor
http://www.dietdoctor.com
Discover Magazine Online
http://discovermagazine.com/
Dr. Bernstein's Diabetes Solution
http://diabetes-book.com/
Dr. Gabe Mirkin
http://www.drmirkin.com/
Dr. Michael R. Eades
http://www.proteinpower.com/drmike
Dr. Nemechek's Integrative Medicine
http://www.nemechekconsultativemedicine.com
Dr. Ron Rosedale
http://www.drrosedale.com/
Entropy Production
http://entropyproduction.blogspot.com/
Ernestine Shepherd
http://ernestineshepherd.net
Evolution for Everyone
http://scienceblogs.com/evolution/
Evolutionary Psychiatry
http://evolutionarypsychiatry.blogspot.com/
Evolving Thoughts by John Wilkins
http://evolvingthoughts.net
Exercise Prescription on the Net
http://www.exrx.net/
Experiments in Lifestyle Design by Tim Ferriss
http://www.fourhourworkweek.com/blog/
Fat Head
http://www.fathead-movie.com/
Fit 2 Fat 2 Fit
http://www.fit2fat2fit.com
Free the Animal
http://freetheanimal.com/
Grassroots Health
http://www.grassrootshealth.net/
Girl Gone Primal
http://girlgoneprimal.blogspot.com/
Gnolls by J. Stanton
http://www.gnolls.org
Health News Review
http://healthnewsreview.org/
Healthcare Epistemocrat
http://epistemocrat.blogspot.com/
Heretic
http://stan-heretic.blogspot.com/
Homo Consumericus
http://www.psychologytoday.com/blog/homo-consumericus
Hunt, Gather, Love
http://huntgatherlove.com/
Hunter Gatherer
http://hunter-gatherer.com/
Hyperlipid
http://high-fat-nutrition.blogspot.com/
ItsTheWooo's The Scribble Pad
http://itsthewooo.blogspot.com/
John Hawks Weblog
http://johnhawks.net/weblog
Julianne's Paleo & Zone Nutrition Blog
http://paleozonenutrition.wordpress.com/
Lean Gains
http://www.leangains.com/
Low-Carb for You
http://lowcarb4u.blogspot.com/
Lucas Tafur
http://www.lucastafur.com
Mark's Daily Apple
http://www.marksdailyapple.com/
Matt Metzgar's Blog
http://www.mattmetzgar.com/
Maxwell Murphy
http://maxwellmurphy.typepad.com/
Metabolism Society
http://nmsociety.org/
Michael Barker's Type 2 Ketosis Prone Diabetes
http://ketosisprone.blogspot.com/
Muscle and the City
http://www.muscleandthecity.com/
MuscleHack
http://www.musclehack.com/
My Carb Sane-Asylum
http://carbsanity.blogspot.com/
My Carb Sane Chronicles
http://carbsanitychronicles.blogspot.com/
Natural Messiah
http://naturalmessiah.blogspot.com/
Nephropal
http://nephropal.blogspot.com/
Nigee's Diet & Nutrition Blog
http://nigeepoo.blogspot.com/
Nourishing by Heart
http://lunchwithouted.wordpress.com/
Nutrition and Physical Regeneration
http://nutrition-and-physical-regeneration.com/blog
Nutrition, Health & Heart Disease
http://www.health-heart.org/
Omega-6 Fat News Commentary
http://omega-6-omega-3-balance.omegaoptimize.com/
Paleo Clinic
http://paleoclinic.blogspot.com/
Paleo Diet
http://paleodiet.com/
Paleo Hacks
http://paleohacks.com/
PaleoFitMD
http://paleofitmd.tumblr.com/
Patrick Ward's Optimum Sports Performance
http://optimumsportsperformance.com/blog/
Pay Now Live Later
http://paynowlivelater.blogspot.com/
Philosophy of Weight Management
http://philosophyofweightmanagement.blogspot.com
Prague Stepchild
http://praguestepchild.blogspot.com/
Primal Montain
http://www.primalmountain.com/c/blog/
Primal Wisdom
http://donmatesz.blogspot.com/
Principle Into Practice
http://principleintopractice.com
Protein Power
http://www.proteinpower.com/
PāNu
http://www.paleonu.com/
Rambling Outside the Box
http://ramblingoutsidethebox.blogspot.com/
Ramblings of a Carnivore
http://ramblingsofacarnivore.blogspot.com/
Raw Food SOS
http://rawfoodsos.com/
Ray Peat
http://raypeat.com/
Robb Wolf
http://robbwolf.com/
Ron Brown's The Myth of Loose Skin
http://www.bodyfatguide.com/LooseSkin.htm
Sandwalk by Laurence Moran
http://sandwalk.blogspot.com
Scooby's Home Bodybuilding Workouts
http://www.scoobysworkshop.com/
Seth Roberts's Blog
http://blog.sethroberts.net
Skyler Tanner
http://skylertanner.com
Sock Doc - Natural Injury Treatment & Prevention
http://sock-doc.com
Son of Grok
http://www.sonofgrok.com/
Spark of Reason
http://sparkofreason.blogspot.com/
Stella Style
http://stellastyle.com/
Survivorman - Discovery
http://dsc.discovery.com/fansites/survivorman/survivorman.html
That Paleo Guy
http://thatpaleoguy.com
The Carnivore Health Weblog
http://www.carnivorehealth.com
The Daily Lipid
http://www.cholesterol-and-health.com/cholesterol-blog.html
The Evolution & Medicine Review
http://evmedreview.com/
The Heart Scan
http://heartscanblog.blogspot.com/
The Healthy Skeptic
http://thehealthyskeptic.org/
The Livin' La Vida Low-Carb Show
http://www.thelivinlowcarbshow.com/shownotes
The Paleo Diet
http://www.thepaleodiet.com/
The Weston A. Price Foundation
http://www.westonaprice.org/
Theory to Practice
http://theorytopractice.wordpress.com/
Vitamin D Council
http://www.vitamindcouncil.org/
Vitamin D Wiki
http://www.vitamindwiki.com/
Weightology
http://weightology.net/
Whole Health Source
http://wholehealthsource.blogspot.com/
Wikipedia - Strength Training
http://en.wikipedia.org/wiki/Strength_training
Wildly Fluctuating
http://wildlyfluctuating.blogspot.com/
Zero Currency, Moneyless World - By Daniel Suelo
http://zerocurrency.blogspot.com/
Zeroing in on Recovery
http://malpaz.wordpress.com/
Zoe Harcombe
http://www.zoeharcombe.com/
180 Degree Health
http://180degreehealth.blogspot.com/
Alan Aragon
http://www.alanaragon.com/
Animal Pharm
http://drbganimalpharm.blogspot.com/
Ancestralize Me!
http://www.ancestralizeme.com/
Anthony Colpo
http://anthonycolpo.com/
Arthur De Vany
http://www.arthurdevany.com/
At Darwin's Table
http://darwinstable.wordpress.com/
Athletics by Nature
http://gregcarver.com/blog
Barefoot Ted's Adventures
http://barefootted.com/
Beef and Whiskey
http://beefandwhiskey.com/
Big Muscles Fast
http://www.bigmusclesfast.com/
Blaine's Low Carb Kitchen
http://fittv.discovery.com/fansites/blaine/recipes/recipes.html
Blood Sugar 101
http://www.phlaunt.com/diabetes
Bob Delmonteque
http://www.bodyrecomposition.com/Brad Pilon's Blog
http://bradpilon.com/
Canibais e Reis
http://www.canibaisereis.com/
Cholesterol and Health
http://www.cholesterol-and-health.com/
Colorado State University's Physiologic Effects of Insulin
http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/pancreas/insulin_phys.html
Conditioning Research
http://conditioningresearch.blogspot.com/
Cooling Inflammation
http://coolinginflammation.blogspot.com/
Cut the Carb
http://www.cutthecarb.com/
David Mendosa
http://www.healthcentral.com/diabetes/c/17
Diabetes Update
http://diabetesupdate.blogspot.com/
Diet Doctor
http://www.dietdoctor.com
Discover Magazine Online
http://discovermagazine.com/
Dr. Bernstein's Diabetes Solution
http://diabetes-book.com/
Dr. Gabe Mirkin
http://www.drmirkin.com/
Dr. Michael R. Eades
http://www.proteinpower.com/drmike
Dr. Nemechek's Integrative Medicine
http://www.nemechekconsultativemedicine.com
Dr. Ron Rosedale
http://www.drrosedale.com/
Entropy Production
http://entropyproduction.blogspot.com/
Ernestine Shepherd
http://ernestineshepherd.net
Evolution for Everyone
http://scienceblogs.com/evolution/
Evolutionary Psychiatry
http://evolutionarypsychiatry.blogspot.com/
Evolving Thoughts by John Wilkins
http://evolvingthoughts.net
Exercise Prescription on the Net
http://www.exrx.net/
Experiments in Lifestyle Design by Tim Ferriss
http://www.fourhourworkweek.com/blog/
Fat Head
http://www.fathead-movie.com/
Fit 2 Fat 2 Fit
http://www.fit2fat2fit.com
Free the Animal
http://freetheanimal.com/
Grassroots Health
http://www.grassrootshealth.net/
Girl Gone Primal
http://girlgoneprimal.blogspot.com/
Gnolls by J. Stanton
http://www.gnolls.org
Health News Review
http://healthnewsreview.org/
Healthcare Epistemocrat
http://epistemocrat.blogspot.com/
Heretic
http://stan-heretic.blogspot.com/
Homo Consumericus
http://www.psychologytoday.com/blog/homo-consumericus
Hunt, Gather, Love
http://huntgatherlove.com/
Hunter Gatherer
http://hunter-gatherer.com/
Hyperlipid
http://high-fat-nutrition.blogspot.com/
ItsTheWooo's The Scribble Pad
http://itsthewooo.blogspot.com/
John Hawks Weblog
http://johnhawks.net/weblog
Julianne's Paleo & Zone Nutrition Blog
http://paleozonenutrition.wordpress.com/
Lean Gains
http://www.leangains.com/
Low-Carb for You
http://lowcarb4u.blogspot.com/
Lucas Tafur
http://www.lucastafur.com
Mark's Daily Apple
http://www.marksdailyapple.com/
Matt Metzgar's Blog
http://www.mattmetzgar.com/
Maxwell Murphy
http://maxwellmurphy.typepad.com/
Metabolism Society
http://nmsociety.org/
Michael Barker's Type 2 Ketosis Prone Diabetes
http://ketosisprone.blogspot.com/
Muscle and the City
http://www.muscleandthecity.com/
MuscleHack
http://www.musclehack.com/
My Carb Sane-Asylum
http://carbsanity.blogspot.com/
My Carb Sane Chronicles
http://carbsanitychronicles.blogspot.com/
Natural Messiah
http://naturalmessiah.blogspot.com/
Nephropal
http://nephropal.blogspot.com/
Nigee's Diet & Nutrition Blog
http://nigeepoo.blogspot.com/
Nourishing by Heart
http://lunchwithouted.wordpress.com/
Nutrition and Physical Regeneration
http://nutrition-and-physical-regeneration.com/blog
Nutrition, Health & Heart Disease
http://www.health-heart.org/
Omega-6 Fat News Commentary
http://omega-6-omega-3-balance.omegaoptimize.com/
Paleo Clinic
http://paleoclinic.blogspot.com/
Paleo Diet
http://paleodiet.com/
Paleo Hacks
http://paleohacks.com/
PaleoFitMD
http://paleofitmd.tumblr.com/
Patrick Ward's Optimum Sports Performance
http://optimumsportsperformance.com/blog/
Pay Now Live Later
http://paynowlivelater.blogspot.com/
Philosophy of Weight Management
http://philosophyofweightmanagement.blogspot.com
Prague Stepchild
http://praguestepchild.blogspot.com/
Primal Montain
http://www.primalmountain.com/c/blog/
Primal Wisdom
http://donmatesz.blogspot.com/
Principle Into Practice
http://principleintopractice.com
Protein Power
http://www.proteinpower.com/
PāNu
http://www.paleonu.com/
Rambling Outside the Box
http://ramblingoutsidethebox.blogspot.com/
Ramblings of a Carnivore
http://ramblingsofacarnivore.blogspot.com/
Raw Food SOS
http://rawfoodsos.com/
Ray Peat
http://raypeat.com/
Robb Wolf
http://robbwolf.com/
Ron Brown's The Myth of Loose Skin
http://www.bodyfatguide.com/LooseSkin.htm
Sandwalk by Laurence Moran
http://sandwalk.blogspot.com
Scooby's Home Bodybuilding Workouts
http://www.scoobysworkshop.com/
Seth Roberts's Blog
http://blog.sethroberts.net
Skyler Tanner
http://skylertanner.com
Sock Doc - Natural Injury Treatment & Prevention
http://sock-doc.com
Son of Grok
http://www.sonofgrok.com/
Spark of Reason
http://sparkofreason.blogspot.com/
Stella Style
http://stellastyle.com/
Survivorman - Discovery
http://dsc.discovery.com/fansites/survivorman/survivorman.html
That Paleo Guy
http://thatpaleoguy.com
The Carnivore Health Weblog
http://www.carnivorehealth.com
The Daily Lipid
http://www.cholesterol-and-health.com/cholesterol-blog.html
The Evolution & Medicine Review
http://evmedreview.com/
The Heart Scan
http://heartscanblog.blogspot.com/
The Healthy Skeptic
http://thehealthyskeptic.org/
The Livin' La Vida Low-Carb Show
http://www.thelivinlowcarbshow.com/shownotes
The Paleo Diet
http://www.thepaleodiet.com/
The Paleo Diet Blog
http://www.westonaprice.org/
Theory to Practice
http://theorytopractice.wordpress.com/
Vitamin D Council
http://www.vitamindcouncil.org/
Vitamin D Wiki
http://www.vitamindwiki.com/
Weightology
http://weightology.net/
Whole Health Source
http://wholehealthsource.blogspot.com/
Wikipedia - Strength Training
http://en.wikipedia.org/wiki/Strength_training
Wildly Fluctuating
http://wildlyfluctuating.blogspot.com/
Zero Currency, Moneyless World - By Daniel Suelo
http://zerocurrency.blogspot.com/
Zeroing in on Recovery
http://malpaz.wordpress.com/
Zoe Harcombe
http://www.zoeharcombe.com/
180 Degree Health
http://180degreehealth.blogspot.com/
Labels:
links
Tuesday, April 20, 2010
What causes Autism
Any connection between autism and childhood vaccines?
I don't really "believe" in much unless backed by science. I realize that the connection of vaccines and autism is a touchy subject and that there are opposing viewpoints. Eventually, however, reason must come into the picture and, despite what our opinions are, we need to rely on evidence to guide decision making.
Just last February, The Lancet retracted the study by Dr. Andrew Wakefield that had linked vaccines with autism. The medical journal cited flaws and unethical activity in connecting autism with vaccines (1). This was the study that had launched the first wave of groups against vaccines like Jenny MccCarthy's Generation Rescue. And I think everyone needs to all get over this and continue to see vaccines for what they are, life-saving medicines.
I know that just discounting vaccines' role in autism is not enough to appease a lot of people who fear for their children. After all, according to the CDC, 1 in 110 children in the U.S. now have autism. If not vaccines, than what is making this happen?
Vitamin D Theory
I, for one (being the vitamin D nut that I am), have high hopes for what's been dubbed the "Vitamin D Theory". The theory suggests that our autism epidemic began at or around the same time as did our epidemic of vitamin D insufficiency (2). If there is a link, then it would explain why there is a higher rate of autism among blacks and there should be a higher rate among children who are not in the sun for sufficient amounts of time.
According to Dr. John Cannell writing in Vitamin D Council's January newsletter, "The 'all autism is caused from vaccinations' crowd cannot accept the Vitamin D possibility as it threatens their core beliefs. They simply cannot change their minds" (3).
Then again, there's not much yet to support the vitamin D link, but Dr. Cannell adds "...organized medicine would say you should stop the vitamin D and watch your son deteriorate, which is why slavery to evidence based medicine is fine for scientists and unethical for practitioners" (3).
References
1. CNN. Medical Journal retracts study linking autism to vaccine. Available at: http://www.cnn.com/2010/HEALTH/02/02/lancet.retraction.autism/index.html
2. Vitamin D Council. http://www.vitamindcouncil.org/health/autism/vit-D-theory-autism.shtml
3. Cannell J. Vitamin D Newsletter. 2010 Jan 30.
I don't really "believe" in much unless backed by science. I realize that the connection of vaccines and autism is a touchy subject and that there are opposing viewpoints. Eventually, however, reason must come into the picture and, despite what our opinions are, we need to rely on evidence to guide decision making.
Just last February, The Lancet retracted the study by Dr. Andrew Wakefield that had linked vaccines with autism. The medical journal cited flaws and unethical activity in connecting autism with vaccines (1). This was the study that had launched the first wave of groups against vaccines like Jenny MccCarthy's Generation Rescue. And I think everyone needs to all get over this and continue to see vaccines for what they are, life-saving medicines.
I know that just discounting vaccines' role in autism is not enough to appease a lot of people who fear for their children. After all, according to the CDC, 1 in 110 children in the U.S. now have autism. If not vaccines, than what is making this happen?
Vitamin D Theory
I, for one (being the vitamin D nut that I am), have high hopes for what's been dubbed the "Vitamin D Theory". The theory suggests that our autism epidemic began at or around the same time as did our epidemic of vitamin D insufficiency (2). If there is a link, then it would explain why there is a higher rate of autism among blacks and there should be a higher rate among children who are not in the sun for sufficient amounts of time.
According to Dr. John Cannell writing in Vitamin D Council's January newsletter, "The 'all autism is caused from vaccinations' crowd cannot accept the Vitamin D possibility as it threatens their core beliefs. They simply cannot change their minds" (3).
Then again, there's not much yet to support the vitamin D link, but Dr. Cannell adds "...organized medicine would say you should stop the vitamin D and watch your son deteriorate, which is why slavery to evidence based medicine is fine for scientists and unethical for practitioners" (3).
References
1. CNN. Medical Journal retracts study linking autism to vaccine. Available at: http://www.cnn.com/2010/HEALTH/02/02/lancet.retraction.autism/index.html
2. Vitamin D Council. http://www.vitamindcouncil.org/health/autism/vit-D-theory-autism.shtml
3. Cannell J. Vitamin D Newsletter. 2010 Jan 30.
Labels:
Autism
Sunday, April 18, 2010
Ketones and Ketosis: Physiological and pathological forms
Ketones are compounds that have a specific chemical structure. The figure below (from: Wikipedia) shows the chemical structure of various types of ketones. As you can see, all ketones share a carbonyl group; that is the “O=” part of their chemical structure. A carbonyl group is an oxygen atom double-bonded to a carbon atom.
Technically speaking, many substances can be classified as ketones. Not all of these are involved in the same metabolic processes in humans. For example, fructose is technically a ketone, but it is not one of the three main ketones produced by humans from dietary macronutrients (discussed below), and is not metabolized in the same way as are those three main ketones.
Humans, as well as most other vertebrates, produce three main ketones (also known as ketone bodies) from dietary macronutrients. These are acetone, acetoacetate and beta-hydroxybutyrate. Low carbohydrate diets tend to promote glycogen depletion, which in turn leads to increased production of these ketones. Glycogen is stored in the liver and muscles. Liver glycogen is used by the body to maintain blood glucose levels within a narrow range in the fasted state. Examples of diets that tend to promote glycogen depletion are the Atkins Diet and Kwaśniewski’s Optimal Diet.
A search for articles on ketosis in scientific databases usually returns a large number of articles dealing with ketosis in cows. Why? The reason is that ketosis reduces milk production, by both reducing the amount of fat and glucose available for milk synthesis. In fact, ketosis is referred to as a “disease” in cows.
In humans, most articles on ketosis refer to pathological ketosis (a.k.a. ketoacidosis), especially in the context of uncontrolled diabetes. One notable exception is an article by Williamson (2005), from which the table below was taken. The table shows ketone concentrations in the blood under various circumstances, in mmol/l.
As you can see, relatively high concentrations of ketones occur in newborn babies (neonate), in adults post-exercise, and in adults fed a high fat diet. Generally speaking, a high fat diet is a low carbohydrate diet, and a high carbohydrate diet is a low fat diet. (One occasionally sees diets that are high in both carbohydrates and fat; which seem excellent at increasing body fat and thus reducing life span. This diet is apparently popular among sumo wrestlers, where genetics and vigorous exercise usually counter the negative diet effects.)
Situations in which ketosis occurs in newborn babies (neonate), in adults post-exercise, and in adults fed a high fat diet are all examples of physiological, or benign, ketosis. Ketones are also found in low concentrations in adults fed a standard American diet.
Ketones are found in very high concentrations in adults with untreated diabetes. This is an example of pathological ketosis, even though ketones are produced as part of a protective compensatory mechanism to spare glucose for the brain and red blood cells (which need glucose to function properly). Pathological ketosis leads to serum ketone levels that can be as much as 80 times (or more) those found in physiological ketosis.
Serum ketone concentrations increase proportionally to decreases in stored glycogen and, when glycogen is low or absent, correlate strongly (and inversely) with blood glucose levels. In some individuals glycogen is practically absent due to a genetic condition that leads to hepatic glycogen synthase deficiency. This is a deficiency of the enzyme that promotes glycogen synthesis by the liver. The figure below (also from Williamson, 2005) shows the variations in glucose and ketone levels in a child with glycogen synthase deficiency.
What happened with this child? Williamson answers this question: “It is of interest that this particular child suffered no ill effects from the daily exposure to high concentrations of ketone bodies, underlining their role as normal substrates for the brain when available.”
Unlike glucose and lipoprotein-bound fats (in VLDL, for example), unused ketones cannot be converted back to substances that can be stored by the body. Thus excess ketones are eliminated in the urine; leading to their detection by various tests, e.g., Ketostix tests. This elimination of unused ketones in the urine is one of the reasons why low carbohydrate diets are believed to lead to enhanced body fat loss.
In summary, ketones are present in the blood most of the time, in most people, whether they are on a ketogenic diet or not. If they do not show up in the urine, it does not mean that they are not present in the blood; although it usually means that their concentration in the blood is not that high. Like glucose, ketones are soluble in water, and thus circulate in the blood without the need for carriers (e.g., albumin, which is needed for the transport of free fatty acids; and VLDL, needed for the transport of triglycerides). Like glucose, they are used as sources of energy by the brain and by muscle tissues.
It has been speculated that ketosis leads to accelerated aging, through the formation of advanced glycation endproducts (AGEs), a speculation that seems to be largely unfounded (see this post). It is difficult to believe that a metabolic process that is universally found in babies and adults post-exercise would have been favored by evolution if it led to accelerated aging.
References:
Williamson, D.H. (2005). Ketosis. Encyclopedia of Human Nutrition, 91-98.
Technically speaking, many substances can be classified as ketones. Not all of these are involved in the same metabolic processes in humans. For example, fructose is technically a ketone, but it is not one of the three main ketones produced by humans from dietary macronutrients (discussed below), and is not metabolized in the same way as are those three main ketones.
Humans, as well as most other vertebrates, produce three main ketones (also known as ketone bodies) from dietary macronutrients. These are acetone, acetoacetate and beta-hydroxybutyrate. Low carbohydrate diets tend to promote glycogen depletion, which in turn leads to increased production of these ketones. Glycogen is stored in the liver and muscles. Liver glycogen is used by the body to maintain blood glucose levels within a narrow range in the fasted state. Examples of diets that tend to promote glycogen depletion are the Atkins Diet and Kwaśniewski’s Optimal Diet.
A search for articles on ketosis in scientific databases usually returns a large number of articles dealing with ketosis in cows. Why? The reason is that ketosis reduces milk production, by both reducing the amount of fat and glucose available for milk synthesis. In fact, ketosis is referred to as a “disease” in cows.
In humans, most articles on ketosis refer to pathological ketosis (a.k.a. ketoacidosis), especially in the context of uncontrolled diabetes. One notable exception is an article by Williamson (2005), from which the table below was taken. The table shows ketone concentrations in the blood under various circumstances, in mmol/l.
As you can see, relatively high concentrations of ketones occur in newborn babies (neonate), in adults post-exercise, and in adults fed a high fat diet. Generally speaking, a high fat diet is a low carbohydrate diet, and a high carbohydrate diet is a low fat diet. (One occasionally sees diets that are high in both carbohydrates and fat; which seem excellent at increasing body fat and thus reducing life span. This diet is apparently popular among sumo wrestlers, where genetics and vigorous exercise usually counter the negative diet effects.)
Situations in which ketosis occurs in newborn babies (neonate), in adults post-exercise, and in adults fed a high fat diet are all examples of physiological, or benign, ketosis. Ketones are also found in low concentrations in adults fed a standard American diet.
Ketones are found in very high concentrations in adults with untreated diabetes. This is an example of pathological ketosis, even though ketones are produced as part of a protective compensatory mechanism to spare glucose for the brain and red blood cells (which need glucose to function properly). Pathological ketosis leads to serum ketone levels that can be as much as 80 times (or more) those found in physiological ketosis.
Serum ketone concentrations increase proportionally to decreases in stored glycogen and, when glycogen is low or absent, correlate strongly (and inversely) with blood glucose levels. In some individuals glycogen is practically absent due to a genetic condition that leads to hepatic glycogen synthase deficiency. This is a deficiency of the enzyme that promotes glycogen synthesis by the liver. The figure below (also from Williamson, 2005) shows the variations in glucose and ketone levels in a child with glycogen synthase deficiency.
What happened with this child? Williamson answers this question: “It is of interest that this particular child suffered no ill effects from the daily exposure to high concentrations of ketone bodies, underlining their role as normal substrates for the brain when available.”
Unlike glucose and lipoprotein-bound fats (in VLDL, for example), unused ketones cannot be converted back to substances that can be stored by the body. Thus excess ketones are eliminated in the urine; leading to their detection by various tests, e.g., Ketostix tests. This elimination of unused ketones in the urine is one of the reasons why low carbohydrate diets are believed to lead to enhanced body fat loss.
In summary, ketones are present in the blood most of the time, in most people, whether they are on a ketogenic diet or not. If they do not show up in the urine, it does not mean that they are not present in the blood; although it usually means that their concentration in the blood is not that high. Like glucose, ketones are soluble in water, and thus circulate in the blood without the need for carriers (e.g., albumin, which is needed for the transport of free fatty acids; and VLDL, needed for the transport of triglycerides). Like glucose, they are used as sources of energy by the brain and by muscle tissues.
It has been speculated that ketosis leads to accelerated aging, through the formation of advanced glycation endproducts (AGEs), a speculation that seems to be largely unfounded (see this post). It is difficult to believe that a metabolic process that is universally found in babies and adults post-exercise would have been favored by evolution if it led to accelerated aging.
References:
Williamson, D.H. (2005). Ketosis. Encyclopedia of Human Nutrition, 91-98.
Friday, April 16, 2010
Thoughts on High Fructose Corn Syrup
There are some really wacked people on the Internet who try to blame the whole obesity epidemic on HFCS, fructose or agave and are misguiding everyone. I liken it to the same misguidance that occurred in 1980s when everyone was scared of fat.
You shouldn't just cut out HCFS and replace it regular sugar or another caloric sweetener. It's really overeating, the overabundance of calories much of it from sugar, that in general contributes to this obesity problem.
What our real problem is is that our brains are wired for fats, carbs and salt that has led us into this obesity crisis now. As a whole, our species needed this wiring to seek out nutritious foods that helped us survive.
But in this modern world of aplenty, the answer to our obesity problem is to control our brains (or trick them with artificial stuff) and use simple discipline, portion control and balanced, nutritious meals.
You shouldn't just cut out HCFS and replace it regular sugar or another caloric sweetener. It's really overeating, the overabundance of calories much of it from sugar, that in general contributes to this obesity problem.
What our real problem is is that our brains are wired for fats, carbs and salt that has led us into this obesity crisis now. As a whole, our species needed this wiring to seek out nutritious foods that helped us survive.
But in this modern world of aplenty, the answer to our obesity problem is to control our brains (or trick them with artificial stuff) and use simple discipline, portion control and balanced, nutritious meals.
Labels:
nutr therap
Thursday, April 15, 2010
Sucralose (Splenda)
Sucralose has been on the market for about two decades now and has been touted as a quite the wonderful artificial sweetener. The safety profile of sucralose has been excellent in adults and it has already helped many with type 2 diabetes to manage blood sugar without having to give up on many of their favorite foods and beverages.
Because of increased use of Sucralose over the years, however, high concentrations of it has been popping up in the environment and there have been worries about how the artificial sweetener may influence infants, children and even animals. One big worry has been potential affects on brain growth.
Two Swedish researchers, Dr Viberg and Dr Fredriksson set out to study the possible neurotoxicity of sucralose in mice. They gave just mice an oral dose of 5-125 mg of sucralose per kilogram bodyweight per day on days 8 through 12 immediately after their birth.
Then, the researchers killed the mice and analyzed their brains. They checked for key proteins and found no alterations that would indicate a disturbance to neuronal development.
Thus, they concluded, sucralose "seems to be a safe alternative for people", and possibly even during pregnancy, as it does not affect growth and development of the brain.
Reference
Viberg H, Fredriksson A. Neonatal exposure to sucralose does not alter biochemical markers of neuronal development or adult behavior. Nutrition. 2010 Jan 27. [Epub ahead of print]
Labels:
nutr therap
High cola intake may cut sperm count, reports Danish study
 Men who drink a few too many Diet Coke or some other cola-like beverages daily may have fewer sperm, according to a new study.
Men who drink a few too many Diet Coke or some other cola-like beverages daily may have fewer sperm, according to a new study.The study, published in the April 15, 2010 issue of American Journal of Epidemiology (1), had examined the semen quality of more than 2,500 young Danish men who had been recruited upon was evaluated for fitness and military service.
They found that those subjects who reported on a questionnaire that they consumed high amounts of caffeine (more than 800 mg per day) or high intakes of cola (more than 14 half-liter bottles per week) had reduced sperm concentration and total sperm count. On the other hand, the consumption of only moderate amounts of caffeine (less than 800 mg per day) or low amounts of cola (less than 14 half-liter bottles per week) were not associated with any similar effect on sperm concentration or count.
There was no association established between caffeine from tea or coffee and influence on sperm count.
The Copenhagen researchers of University of Denmark of Growth and Reproduction concluded that they "cannot exclude the possibility of a threshold above which cola, and possibly caffeine, negatively affects semen quality" (1).
They added, "Alternatively, the less healthy lifestyle of these men may explain these findings" (1).
Still, if you're interested in maintaining your vitality (who isn't?), it may be better to avoid the cola!
Caffeine and Semen Quality
There have been several studies that have investigated caffeine and a possible association with semen quality, which have led to conflicting results.
Previous to this study on high intakes of cola, there had been a pregnancy cohort in 2008 on more than 5,000 males that evaluated semen quality in association with prenatal coffee and caffeine exposure (2).
The study, also from Denmark, found that although high caffeine intake didn't have any significant effect on semen quality, it did lead to increased testosterone concentrations (approximately 14 percent) in the men (2).
So, until more research is conducted, there's still no need to give up on the coffee.
References
1. Jensen TK, Swan SH, Skakkebaek NE, Rasmussen S, Jørgensen N. Caffeine intake and semen quality in a population of 2,554 young Danish men. Am J Epidemiol. 2010 Apr 15;171(8):883-91. Epub 2010 Mar 25.
2. Ramlau-Hansen CH, Thulstrup AM, Bonde JP, Olsen J, Bech BH. Semen quality according to prenatal coffee and present caffeine exposure: two decades of follow-up of a pregnancy cohort. Hum Reprod. 2008 Dec;23(12):2799-805. Epub 2008 Aug 28.
The Copenhagen researchers of University of Denmark of Growth and Reproduction concluded that they "cannot exclude the possibility of a threshold above which cola, and possibly caffeine, negatively affects semen quality" (1).
They added, "Alternatively, the less healthy lifestyle of these men may explain these findings" (1).
Still, if you're interested in maintaining your vitality (who isn't?), it may be better to avoid the cola!
Caffeine and Semen Quality
There have been several studies that have investigated caffeine and a possible association with semen quality, which have led to conflicting results.
Previous to this study on high intakes of cola, there had been a pregnancy cohort in 2008 on more than 5,000 males that evaluated semen quality in association with prenatal coffee and caffeine exposure (2).
The study, also from Denmark, found that although high caffeine intake didn't have any significant effect on semen quality, it did lead to increased testosterone concentrations (approximately 14 percent) in the men (2).
So, until more research is conducted, there's still no need to give up on the coffee.
References
1. Jensen TK, Swan SH, Skakkebaek NE, Rasmussen S, Jørgensen N. Caffeine intake and semen quality in a population of 2,554 young Danish men. Am J Epidemiol. 2010 Apr 15;171(8):883-91. Epub 2010 Mar 25.
2. Ramlau-Hansen CH, Thulstrup AM, Bonde JP, Olsen J, Bech BH. Semen quality according to prenatal coffee and present caffeine exposure: two decades of follow-up of a pregnancy cohort. Hum Reprod. 2008 Dec;23(12):2799-805. Epub 2008 Aug 28.
Labels:
nutr therap
Luo han guo - a source of xylitol
Louo han guo is a fruit that has been recently hyped up and marketed as a natural sweetener. What is it really? It's really just a source of xylitol. Xylitol is a natural sugar alcohol, which is not digested as easily by the body lending fewer calories per gram than regular sugar. The polyol also has a slight cooling effect, which you would recognize while eating sugarless gum like Trident.
Xylitol was first discovered and isolated in Sweden from birch bark. It is also now widely used in Sweden (where it was first isolated) and used in all sorts of candies there.
Regular use of xylitol is associated with significant reduction of cavities and tooth remineralization (1). Why? Because research shows that xylitol doesn't contribute to tooth decay and, unlike other sugar alcohols like erythritol, it may even help fight cavities by a mechanism of confusing cavity-causing bacteria to eat it and basically die.
Reference
1. Mäkinen KK. Sugar alcohols, caries incidence, and remineralization of caries lesions: a literature review. Int J Dent. 2010;2010:981072. Epub 2010 Jan 5.
Xylitol was first discovered and isolated in Sweden from birch bark. It is also now widely used in Sweden (where it was first isolated) and used in all sorts of candies there.
Regular use of xylitol is associated with significant reduction of cavities and tooth remineralization (1). Why? Because research shows that xylitol doesn't contribute to tooth decay and, unlike other sugar alcohols like erythritol, it may even help fight cavities by a mechanism of confusing cavity-causing bacteria to eat it and basically die.
Reference
1. Mäkinen KK. Sugar alcohols, caries incidence, and remineralization of caries lesions: a literature review. Int J Dent. 2010;2010:981072. Epub 2010 Jan 5.
Labels:
nutr therap
Summing up Low-carb
Low-carbohydrate diets may do wonders for quick weight loss (mostly from water loss) and to improve glucose and insulin levels, but they are not without their adverse effects (1-2).
The body needs carbs for energy. Without sufficient amounts, muscle catabolism and protein will result, the break down of fat stores for fuel will result in incomplete fat oxidation, and an excess of acidic ketones will be produced. Diets too low in carbs can lead to ketoacidosis (1).
However, moderately low-carb diets such as the Mediterranean diet, which includes plenty of fruits, vegetables and monounsatured oils are a good choice for long-term health (2).
References
1. Nix, S. (2005). Williams' Basic Nutrition & Diet Therapy. Philadelphia: Mosby.
2. Shai, I., Schwarzfuchs, D., Yaakov, H., Sahar, D.R., Witkow, S., et al. (July, 2008). Weight loss with a low-carbohydrate, Mediterranean or low-fat diet. The New England Journal of Medicine, 359:229-241.
The body needs carbs for energy. Without sufficient amounts, muscle catabolism and protein will result, the break down of fat stores for fuel will result in incomplete fat oxidation, and an excess of acidic ketones will be produced. Diets too low in carbs can lead to ketoacidosis (1).
However, moderately low-carb diets such as the Mediterranean diet, which includes plenty of fruits, vegetables and monounsatured oils are a good choice for long-term health (2).
References
1. Nix, S. (2005). Williams' Basic Nutrition & Diet Therapy. Philadelphia: Mosby.
2. Shai, I., Schwarzfuchs, D., Yaakov, H., Sahar, D.R., Witkow, S., et al. (July, 2008). Weight loss with a low-carbohydrate, Mediterranean or low-fat diet. The New England Journal of Medicine, 359:229-241.
Labels:
nutr therap
Insulin responses to foods rich in carbohydrates and protein
Insulin is often presented as a hormone that is at the core of the diseases of civilization, particularly because of the insulin response elicited by foods rich in refined carbohydrates and sugars. What is often not mentioned is that protein also elicits an insulin response and so do foods where carbohydrates are mixed with fat. Sometimes the insulin responses are way more than one would expect based on the macronutrient compositions of the foods.
Holt et al. (1997; full reference at the end of this post) conducted a classic study of insulin responses. This study has been widely cited, and paints an interesting picture of differences in insulin responses to various foods. But you have to be careful where you look. There has been some confusion about the results because of the way they are often reported in places like Wikipedia and on various Internet sites that refer to the study.
The key thing to bear in mind when reviewing this study is that the amounts of food used were designed to have the same calorie content: 1000 kJ or 240 kcal (i.e., 240 calories). This led to wild variations in the size of the portions that are compared and their weight in grams. Also, some of the food portions are probably not what people usually eat in one sitting.
In Holt et al.’s (1997) study the participants were 41 lean and healthy university students. They were fed 1000 kJ (240 kcal) portions of the test foods on separate mornings after a 10-hour fast overnight. Blood insulin levels were measured at different times within a 120-minute period after each meal. An insulin score was then calculated from the area under the insulin response curve for each food; white bread was used as the reference food.
Part of Table 2 on page 1267 is shown below (the full text version of the paper is linked at the end of this post), just to illustrate the types and amounts of food served, and the macronutrient breakdown for each food. I hope you can see what I meant when I said that some of the food portions are probably not what people usually eat in one sitting. I don’t think it would be hard to find someone who would eat 158 g of beef steak in one sitting, but 333 g of fish is a little more difficult. Fish has a higher proportion of protein than beef steak, and thus is more satiating. The same goes for 625 g of orange, about 6 oranges. Foods that have more fat have more calories per gram; hence the smaller portions served for high-fat foods.
Table 4 of the article is a bit long, so I am providing it in two parts below. AUC stands for “area under the curve”. As you can see, for isocaloric portions of different foods (i.e., with the same amount of calories), there is a huge variation in insulin response. The insulin AUCs are shown on the second numeric column from the left. Also note that the insulin responses (AUC) for white bread varied in different meals. This complicates things a bit, but at least provides a more realistic view of the responses since each participant served as his or her own control.
Look at the third column from the right, which shows the insulin responses per gram of each food, compared with the response to white bread, always shown at the top for each group of related foods (e.g., protein-rich foods). The gram-adjusted response for whole-meal bread is rather high, and so is the glucose response. The gram-adjusted insulin response to potatoes is less than one-third of the response to white bread, even though the non-gram-adjusted glucose response is higher. The insulin response to beef is also less than one-third of the response to white bread, gram-for-gram. Even cheese leads to a gram-adjusted response that is about half the one for white bread, and I don’t think many people will eat the same amount of cheese in one sitting as they would do with white bread.
In summary, insulin responses to protein-rich foods are often 50 to 70 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods. Also, insulin responses to unrefined carbohydrate-rich foods (e.g., potato, fruits) are often 70 to 90 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods.
Why do insulin levels go up in response to dietary protein?
One of the reasons is that insulin is needed for tissue protein synthesis. That is, increased circulating protein (as amino acids) and insulin have a net anabolic effect, promoting muscle growth and inhibiting muscle breakdown. (Muscle protein synthesis and breakdown happen all the time; the net effect defines whether muscle grows or shrinks.) In this respect, insulin acts in conjunction with other hormones, such as growth hormone and insulin-like growth factor 1.
Reference:
Holt, S.H., Miller, J.C., & Petocz, P. (1997). An insulin index of foods: The insulin demand generated by 1000-kJ portions of common foods. American Journal of Clinical Nutrition, 66, 1264-1276.
Holt et al. (1997; full reference at the end of this post) conducted a classic study of insulin responses. This study has been widely cited, and paints an interesting picture of differences in insulin responses to various foods. But you have to be careful where you look. There has been some confusion about the results because of the way they are often reported in places like Wikipedia and on various Internet sites that refer to the study.
The key thing to bear in mind when reviewing this study is that the amounts of food used were designed to have the same calorie content: 1000 kJ or 240 kcal (i.e., 240 calories). This led to wild variations in the size of the portions that are compared and their weight in grams. Also, some of the food portions are probably not what people usually eat in one sitting.
In Holt et al.’s (1997) study the participants were 41 lean and healthy university students. They were fed 1000 kJ (240 kcal) portions of the test foods on separate mornings after a 10-hour fast overnight. Blood insulin levels were measured at different times within a 120-minute period after each meal. An insulin score was then calculated from the area under the insulin response curve for each food; white bread was used as the reference food.
Part of Table 2 on page 1267 is shown below (the full text version of the paper is linked at the end of this post), just to illustrate the types and amounts of food served, and the macronutrient breakdown for each food. I hope you can see what I meant when I said that some of the food portions are probably not what people usually eat in one sitting. I don’t think it would be hard to find someone who would eat 158 g of beef steak in one sitting, but 333 g of fish is a little more difficult. Fish has a higher proportion of protein than beef steak, and thus is more satiating. The same goes for 625 g of orange, about 6 oranges. Foods that have more fat have more calories per gram; hence the smaller portions served for high-fat foods.
Table 4 of the article is a bit long, so I am providing it in two parts below. AUC stands for “area under the curve”. As you can see, for isocaloric portions of different foods (i.e., with the same amount of calories), there is a huge variation in insulin response. The insulin AUCs are shown on the second numeric column from the left. Also note that the insulin responses (AUC) for white bread varied in different meals. This complicates things a bit, but at least provides a more realistic view of the responses since each participant served as his or her own control.
Look at the third column from the right, which shows the insulin responses per gram of each food, compared with the response to white bread, always shown at the top for each group of related foods (e.g., protein-rich foods). The gram-adjusted response for whole-meal bread is rather high, and so is the glucose response. The gram-adjusted insulin response to potatoes is less than one-third of the response to white bread, even though the non-gram-adjusted glucose response is higher. The insulin response to beef is also less than one-third of the response to white bread, gram-for-gram. Even cheese leads to a gram-adjusted response that is about half the one for white bread, and I don’t think many people will eat the same amount of cheese in one sitting as they would do with white bread.
In summary, insulin responses to protein-rich foods are often 50 to 70 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods. Also, insulin responses to unrefined carbohydrate-rich foods (e.g., potato, fruits) are often 70 to 90 percent lower than responses to equivalent amounts of refined carbohydrate-rich foods.
Why do insulin levels go up in response to dietary protein?
One of the reasons is that insulin is needed for tissue protein synthesis. That is, increased circulating protein (as amino acids) and insulin have a net anabolic effect, promoting muscle growth and inhibiting muscle breakdown. (Muscle protein synthesis and breakdown happen all the time; the net effect defines whether muscle grows or shrinks.) In this respect, insulin acts in conjunction with other hormones, such as growth hormone and insulin-like growth factor 1.
Reference:
Holt, S.H., Miller, J.C., & Petocz, P. (1997). An insulin index of foods: The insulin demand generated by 1000-kJ portions of common foods. American Journal of Clinical Nutrition, 66, 1264-1276.
Tuesday, April 13, 2010
Long-term adherence to Dr. Kwaśniewski’s Optimal Diet: Healthy with high LDL cholesterol
This is a study (Grieb, P. et al., 2008; full reference at the end of this post) that I read a few years ago, right after it came out, and at the time I recall thinking about the apparent contradiction between the positive effects of the Optimal Diet and the very elevated LDL cholesterol levels among the participants. I say “contradiction” because of the established and misguided dogma among medical doctors, particularly general practitioners, that decreasing LDL cholesterol levels is the best strategy to avoid cardiovascular disease.
The Optimal Diet is one of the best examples of a healthy diet where LDL cholesterol levels are generally high, in fact much higher than most people are willing to accept as healthy today. (In this study, LDL cholesterol levels were calculated based on the Friedewald equation.)
It is not uncommon to see people concerned about their high LDL cholesterol levels after adopting a low carbohydrate diet. (A low carbohydrate diet is, generally speaking, a high fat diet.) This study shows that this is a rather common thing, and also that it is not something that those who experience it should be too concerned about. To be convinced of this, one can always do a VAP test (see this post for a link to a sample VAP test report) and check his or her LDL particle pattern.
The study presents the Optimal Diet as the Polish equivalent to the Atkins diet. It states that the Diet’s main characteristic is maintaining the proportion of proteins:fat:carbs. in the range of 1:2.5-3.5:0.5, with no restriction on the amount of food consumed. In fact, as you will see in this post, more than 70 percent of the calories consumed by the study participants came from fat.
Easily digestible carbohydrate-rich foods are not part of the Optimal Diet. More specifically, the following foods were listed as not being allowed in the Optimal Diet: sucrose, sweets, honey, jam, white rice, bread, starches in general, beans, potatoes (only in small amounts), and sweetened drinks. Also, the Optimal Diet is definitely a low carbohydrate diet, but not what is often referred to as a "very low carbohydrate diet". In this study, the typical carbohydrate intake per day was around 60 g.
Thirty-one healthy people participated in the study, 17 women and 14 men. The average age was 51.7 (standard deviation: 16.6). They had self-reportedly adhered to the Optimal Diet for at least 1 year prior to the study; the average period of adherence was 4.1 years (standard deviation: 1.9). So, the vast majority had been on the diet for more than 2.2 years, about half for 4.1 years or more, and about one-sixth for more than 6 years. (Check this post if you want to know how these figures can be calculated based on the average period of adherence and the standard deviation.)
The table below (click on it to enlarge) shows anthropometric and physiologic characteristics of the participants. Note that longer adherence to the Optimal Diet (right end of the table) was associated with lower systolic and diastolic blood pressure, as well as lower body mass index (BMI). (It was also associated with lower height and BMR, so I am guessing that more women tended to be long-term adherers than men.) Most of the participants had BMIs in the normal range, with only one in the obese category. That was a 43-year-old man who followed the diet for 1.5 years; he had a BMI of 34.1.
The macronutrient distribution of the Optimal Diet is shown on the table below (click on it to enlarge), as followed by the participants. As you can see, protein intake was not that high; about 53.9 g per day on average for men, a bit less for women. Note the percentage of calories from fat: more than 77 percent for men and 72 percent for women. Given the BMIs just discussed, one can safely say based on this that eating a lot of fat did not make the participants fat.
The table below (click on it to enlarge) has some interesting health markers. Note that free fatty acids (FFAs) were elevated. This is to be expected, as these folks were burning fat for energy most of the time, and not as much glucose. The FFAs are not really “free”, but bound to a protein called albumin, which is abundant in human blood. FFAs yield large quantities of adenosine triphosphate (ATP), the main energy “currency” used by the body.
These levels of FFAs are also usually associated with mild ketosis, where ketones are produced by the body and used for energy. Unlike albumin-bound FFAs, ketones are soluble in water, and thus circulate freely through the blood. The mild ketosis experienced by the participants was possibly to the point where ketones showed in the urine. The article mentions this, and provides a measure of beta-HB (beta-hydroxybutyrate, a ketone body), which is elevated as expected, but does not provide urine or other blood ketone measures (e.g., blood acetone levels). Also note the fairly healthy fasting glucose levels, slightly higher in men than in women, but fairly low overall. Fairly healthy insulin levels as well; at the high end of what Stephan at Whole Health Source would recommend, but still significantly lower than the average insulin level in the U.S. at the time of the article's publication.
Finally, the table below (click on it to enlarge) shows lipids and a few other measures. Total cholesterol was on average a bit more than 278 mg/dL. LDL cholesterol was a bit higher than 188 mg/dL on average; high enough to make most doctors cringe today. Based on the means and standard deviations provided, we can estimate that about 16 percent of the participants had LDL cholesterol levels higher than 228.1 mg/dL. About 2.5 percent of the participants had LDL cholesterol levels higher than 268 mg/dL. And this is all after adhering to the diet for a relatively long period of time; even higher LDL cholesterol levels might have occurred right after adoption.
Yet average HDL cholesterol was a very high and protective 71.6 mg/dL. This high HDL and the relatively low triglycerides suggest a large-buoyant non-atherogenic LDL particle pattern.
Average HOMA(IR), a measure of insulin resistance, was a low 1.35 mU/mmol; strongly indicating, together with the relatively low fasting glucose levels, that the participants were far from being pre-diabetic, let alone diabetic.
Diabetes is a strong risk factor for cardiovascular disease, and many other health complications; much more so than elevated LDL cholesterol.
The Optimal Diet does not seem to be a diet for bodybuilders, but I would say that, overall, Peter at Hyperlipid has chosen a diet that makes some sense.
Reference:
Grieb, P. et al. (2008). Long-term consumption of a carbohydrate-restricted diet does not induce deleterious metabolic effects. Nutrition Research, 28(12), 825-833.
The Optimal Diet is one of the best examples of a healthy diet where LDL cholesterol levels are generally high, in fact much higher than most people are willing to accept as healthy today. (In this study, LDL cholesterol levels were calculated based on the Friedewald equation.)
It is not uncommon to see people concerned about their high LDL cholesterol levels after adopting a low carbohydrate diet. (A low carbohydrate diet is, generally speaking, a high fat diet.) This study shows that this is a rather common thing, and also that it is not something that those who experience it should be too concerned about. To be convinced of this, one can always do a VAP test (see this post for a link to a sample VAP test report) and check his or her LDL particle pattern.
The study presents the Optimal Diet as the Polish equivalent to the Atkins diet. It states that the Diet’s main characteristic is maintaining the proportion of proteins:fat:carbs. in the range of 1:2.5-3.5:0.5, with no restriction on the amount of food consumed. In fact, as you will see in this post, more than 70 percent of the calories consumed by the study participants came from fat.
Easily digestible carbohydrate-rich foods are not part of the Optimal Diet. More specifically, the following foods were listed as not being allowed in the Optimal Diet: sucrose, sweets, honey, jam, white rice, bread, starches in general, beans, potatoes (only in small amounts), and sweetened drinks. Also, the Optimal Diet is definitely a low carbohydrate diet, but not what is often referred to as a "very low carbohydrate diet". In this study, the typical carbohydrate intake per day was around 60 g.
Thirty-one healthy people participated in the study, 17 women and 14 men. The average age was 51.7 (standard deviation: 16.6). They had self-reportedly adhered to the Optimal Diet for at least 1 year prior to the study; the average period of adherence was 4.1 years (standard deviation: 1.9). So, the vast majority had been on the diet for more than 2.2 years, about half for 4.1 years or more, and about one-sixth for more than 6 years. (Check this post if you want to know how these figures can be calculated based on the average period of adherence and the standard deviation.)
The table below (click on it to enlarge) shows anthropometric and physiologic characteristics of the participants. Note that longer adherence to the Optimal Diet (right end of the table) was associated with lower systolic and diastolic blood pressure, as well as lower body mass index (BMI). (It was also associated with lower height and BMR, so I am guessing that more women tended to be long-term adherers than men.) Most of the participants had BMIs in the normal range, with only one in the obese category. That was a 43-year-old man who followed the diet for 1.5 years; he had a BMI of 34.1.
The macronutrient distribution of the Optimal Diet is shown on the table below (click on it to enlarge), as followed by the participants. As you can see, protein intake was not that high; about 53.9 g per day on average for men, a bit less for women. Note the percentage of calories from fat: more than 77 percent for men and 72 percent for women. Given the BMIs just discussed, one can safely say based on this that eating a lot of fat did not make the participants fat.
The table below (click on it to enlarge) has some interesting health markers. Note that free fatty acids (FFAs) were elevated. This is to be expected, as these folks were burning fat for energy most of the time, and not as much glucose. The FFAs are not really “free”, but bound to a protein called albumin, which is abundant in human blood. FFAs yield large quantities of adenosine triphosphate (ATP), the main energy “currency” used by the body.
These levels of FFAs are also usually associated with mild ketosis, where ketones are produced by the body and used for energy. Unlike albumin-bound FFAs, ketones are soluble in water, and thus circulate freely through the blood. The mild ketosis experienced by the participants was possibly to the point where ketones showed in the urine. The article mentions this, and provides a measure of beta-HB (beta-hydroxybutyrate, a ketone body), which is elevated as expected, but does not provide urine or other blood ketone measures (e.g., blood acetone levels). Also note the fairly healthy fasting glucose levels, slightly higher in men than in women, but fairly low overall. Fairly healthy insulin levels as well; at the high end of what Stephan at Whole Health Source would recommend, but still significantly lower than the average insulin level in the U.S. at the time of the article's publication.
Finally, the table below (click on it to enlarge) shows lipids and a few other measures. Total cholesterol was on average a bit more than 278 mg/dL. LDL cholesterol was a bit higher than 188 mg/dL on average; high enough to make most doctors cringe today. Based on the means and standard deviations provided, we can estimate that about 16 percent of the participants had LDL cholesterol levels higher than 228.1 mg/dL. About 2.5 percent of the participants had LDL cholesterol levels higher than 268 mg/dL. And this is all after adhering to the diet for a relatively long period of time; even higher LDL cholesterol levels might have occurred right after adoption.
Yet average HDL cholesterol was a very high and protective 71.6 mg/dL. This high HDL and the relatively low triglycerides suggest a large-buoyant non-atherogenic LDL particle pattern.
Average HOMA(IR), a measure of insulin resistance, was a low 1.35 mU/mmol; strongly indicating, together with the relatively low fasting glucose levels, that the participants were far from being pre-diabetic, let alone diabetic.
Diabetes is a strong risk factor for cardiovascular disease, and many other health complications; much more so than elevated LDL cholesterol.
The Optimal Diet does not seem to be a diet for bodybuilders, but I would say that, overall, Peter at Hyperlipid has chosen a diet that makes some sense.
Reference:
Grieb, P. et al. (2008). Long-term consumption of a carbohydrate-restricted diet does not induce deleterious metabolic effects. Nutrition Research, 28(12), 825-833.
Sunday, April 11, 2010
Does low-calorie dieting cause you to "yo yo" because of lowered metabolism?
This post came out of a question from someone who asked a question related to whether or not eating a very low calorie diet would lead to a "yo yo" effect caused by lowered metabolism, stoping weight loss and causing weight gain upon eating normally again.
There is no evidence suggesting that a "yo yo" effect would occur from low-calorie dieting, nor would lowering calories too far "stop" weight loss altogether. Truth is, calorie restriction does reduce metabolic rate, you would lose weight at a rate that is lower than normally expected, but if you started eating normally again, your metabolism would speed back up again.
In 2006, Heilbronn et al. studied the effects of calorie restriction (CR) on metabolism. The researchers published in JAMA the results of a six-month randomized controlled trial on CR and how it made an impact on biomarkers of metabolism as well as longevity and oxidative stress in overweight adults.
The subjects were paid and placed in one of the following groups: a control group, a CR group (25% reduction from baseline), a CR group with exercise (12.5% reduction, 12.5% increase activity), and what they called a very-calorie diet (890 kcal/d) followed by weight management at 15 percent weight reduction.
By the third month, metabolism had slowed (measured in part with plasma T3 levels) in both CR and very low-calorie diets. At six months, metabolism had slowed in the CR, CR with exercise, and very low-calorie diet groups.
Everyone lost weight in the intervention groups. Those on the very-low calorie diet lost the most, but they also lost the most muscle. From that same study, the researchers were the first to find reduced oxidative stress and DNA damage from CR in humans.
So, what do we know? We know that if you also drop even to 500-800 kcal per day that, despite slower metabolism (your body's survival mechanism), you still would lose weight albeit at a lower rate (as stated before).
What some researchers have tried to do since then to "trick" the body to not slow metabolism. They do it by staggering the calories with alternate-day CR/fasting or intermittent CR/fasting. These are interesting topics of research and may show up as new weight-loss fads of the future.
I don't recommend people drop calories or lose weight too quickly because it leads to too much loss of hard-earned muscle and, possibly, gallstones (if you're not drinking enough water and eating small meals throughout the day). In my experience, I've also seen quite a few people go lower than 800 calories per day for weeks and end up without energy, getting sick and looking pretty frail.
It's best, I think, to stick with losing only 1-2 pounds per week (by dropping calories steadily and increasing activity to keep muscle up) and then eventually keeping diet within 800-1200 kcal/d range.
There is no evidence suggesting that a "yo yo" effect would occur from low-calorie dieting, nor would lowering calories too far "stop" weight loss altogether. Truth is, calorie restriction does reduce metabolic rate, you would lose weight at a rate that is lower than normally expected, but if you started eating normally again, your metabolism would speed back up again.
In 2006, Heilbronn et al. studied the effects of calorie restriction (CR) on metabolism. The researchers published in JAMA the results of a six-month randomized controlled trial on CR and how it made an impact on biomarkers of metabolism as well as longevity and oxidative stress in overweight adults.
The subjects were paid and placed in one of the following groups: a control group, a CR group (25% reduction from baseline), a CR group with exercise (12.5% reduction, 12.5% increase activity), and what they called a very-calorie diet (890 kcal/d) followed by weight management at 15 percent weight reduction.
By the third month, metabolism had slowed (measured in part with plasma T3 levels) in both CR and very low-calorie diets. At six months, metabolism had slowed in the CR, CR with exercise, and very low-calorie diet groups.
Everyone lost weight in the intervention groups. Those on the very-low calorie diet lost the most, but they also lost the most muscle. From that same study, the researchers were the first to find reduced oxidative stress and DNA damage from CR in humans.
So, what do we know? We know that if you also drop even to 500-800 kcal per day that, despite slower metabolism (your body's survival mechanism), you still would lose weight albeit at a lower rate (as stated before).
What some researchers have tried to do since then to "trick" the body to not slow metabolism. They do it by staggering the calories with alternate-day CR/fasting or intermittent CR/fasting. These are interesting topics of research and may show up as new weight-loss fads of the future.
I don't recommend people drop calories or lose weight too quickly because it leads to too much loss of hard-earned muscle and, possibly, gallstones (if you're not drinking enough water and eating small meals throughout the day). In my experience, I've also seen quite a few people go lower than 800 calories per day for weeks and end up without energy, getting sick and looking pretty frail.
It's best, I think, to stick with losing only 1-2 pounds per week (by dropping calories steadily and increasing activity to keep muscle up) and then eventually keeping diet within 800-1200 kcal/d range.
Undigested meat in the colon
When you have undigested meat proteins in your colon, they will basically do what they do when thery are outside the colon: they rot. The rotting, or decay, is characterized by a release of foul-smelling chemicals.
One such chemical is cadaverine--the same that gave "cadavers" their name because of the smell they emit--which is the result of protein hydrolysis or the decarboxylation product of lysine. It's similar in structure to putrescine, putrescine itself produced from rotting activity.
Rotting flesh in the colon gives off a horrible odor and the smelly chemicals can become apparent in a person's breath, feces or urine. The person may suffer from the foul odors for a good while as the long process digestion or elimination of the meat continues.
To help speed things along, it's important to maintain a diet high in dietary fiber, specifically insoluble fiber, which helps increase rate of transit in the colon. Insoluble fiber comes from the "woody" parts of plants such as wheat bran and vegetable skins.
No one should have to put up with "the smell of death" after a meal. To avoid offensive gas and bad breath, just eat smaller portions of meat and be sure to also include some salad and extra vegetables.
Reference
Lecture notes by Albert Grazia, M.S.
One such chemical is cadaverine--the same that gave "cadavers" their name because of the smell they emit--which is the result of protein hydrolysis or the decarboxylation product of lysine. It's similar in structure to putrescine, putrescine itself produced from rotting activity.
Rotting flesh in the colon gives off a horrible odor and the smelly chemicals can become apparent in a person's breath, feces or urine. The person may suffer from the foul odors for a good while as the long process digestion or elimination of the meat continues.
To help speed things along, it's important to maintain a diet high in dietary fiber, specifically insoluble fiber, which helps increase rate of transit in the colon. Insoluble fiber comes from the "woody" parts of plants such as wheat bran and vegetable skins.
No one should have to put up with "the smell of death" after a meal. To avoid offensive gas and bad breath, just eat smaller portions of meat and be sure to also include some salad and extra vegetables.
Reference
Lecture notes by Albert Grazia, M.S.
Labels:
nutr therap
The Friedewald and Iranian equations: Fasting triglycerides can seriously distort calculated LDL
Standard lipid profiles provide LDL cholesterol measures based on equations that usually have the following as their inputs (or independent variables): total cholesterol, HDL cholesterol, and triglycerides.
Yes, LDL cholesterol is not measured directly in standard lipid profile tests! This is indeed surprising, since cholesterol-lowering drugs with negative side effects are usually prescribed based on estimated (or "fictitious") LDL cholesterol levels.
The most common of these equations is the Friedewald equation. Through the Friedewald equation, LDL cholesterol is calculated as follows (where TC = total cholesterol, and TG = triglycerides). The inputs and result are in mg/dl.
LDL = TC – HDL – TG / 5
Here is one of the problems with the Friedewald equation. Let us assume that an individual has the following lipid profile numbers: TC = 200, HDL = 50, and trigs. = 150. The calculated LDL will be 120. Let us assume that this same individual reduces triglycerides to 50, from the previous 150, keeping all of the other measures constant. This is a major improvement. However, the calculated LDL will now be 140, and a doctor will tell this person to consider taking statins!
There is evidence that, for individuals with low fasting triglycerides, a more precise equation is one that has come to be known as the “Iranian equation”. The equation has been proposed by Iranian researchers in an article published in the Archives of Iranian Medicine (Ahmadi et al., 2008), hence its nickname. Through the Iranian equation, LDL is calculated as follows. Again, the inputs and result are in mg/dl.
LDL = TC / 1.19 + TG / 1.9 – HDL / 1.1 – 38
The Iranian equation is based on linear regression modeling, which is a good sign, although I would have liked it even better if it was based on nonlinear regression modeling. The reason is that relationships between variables describing health-related phenomena are often nonlinear, leading to biased linear estimations. With a good nonlinear analysis algorithm, a linear relationship will also be captured; that is, the “curve” that describes the relationship will default to a line if the relationship is truly linear (see: warppls.com).
Anyway, an online calculator that implements both equations (Friedewald and Iranian) is linked here; it was the top Google hit on a search for “Iranian equation LDL” at the time of this post’s writing.
As you will see if you try it, the online calculator linked above is useful in showing the difference in calculated LDL cholesterol, using both equations, when fasting triglycerides are very low (e.g., below 50).
The Iranian equation yields high values of LDL cholesterol when triglycerides are high; much higher than those generated by the Friedewald equation. If those are not overestimations (and there is some evidence that, if they are, it is not by much), they describe an alarming metabolic pattern, because high triglycerides are associated with small-dense LDL particles. These particles are the most potentially atherogenic of the LDL particles, in the presence of other factors such as chronic inflammation.
In other words, the Iranian equation gives a clearer idea than the Friedewald equation about the negative health effects of high triglycerides. You need a large number of small-dense LDL particles to carry a high amount of LDL cholesterol.
An even more precise measure of LDL particle configuration is the VAP test; this post has a link to a PDF file with a sample VAP test report.
Reference:
Ahmadi SA, Boroumand MA, Gohari-Moghaddam K, Tajik P, Dibaj SM. (2008). The impact of low serum triglyceride on LDL-cholesterol estimation. Archives of Iranian Medicine, 11(3), 318-21.
Yes, LDL cholesterol is not measured directly in standard lipid profile tests! This is indeed surprising, since cholesterol-lowering drugs with negative side effects are usually prescribed based on estimated (or "fictitious") LDL cholesterol levels.
The most common of these equations is the Friedewald equation. Through the Friedewald equation, LDL cholesterol is calculated as follows (where TC = total cholesterol, and TG = triglycerides). The inputs and result are in mg/dl.
LDL = TC – HDL – TG / 5
Here is one of the problems with the Friedewald equation. Let us assume that an individual has the following lipid profile numbers: TC = 200, HDL = 50, and trigs. = 150. The calculated LDL will be 120. Let us assume that this same individual reduces triglycerides to 50, from the previous 150, keeping all of the other measures constant. This is a major improvement. However, the calculated LDL will now be 140, and a doctor will tell this person to consider taking statins!
There is evidence that, for individuals with low fasting triglycerides, a more precise equation is one that has come to be known as the “Iranian equation”. The equation has been proposed by Iranian researchers in an article published in the Archives of Iranian Medicine (Ahmadi et al., 2008), hence its nickname. Through the Iranian equation, LDL is calculated as follows. Again, the inputs and result are in mg/dl.
LDL = TC / 1.19 + TG / 1.9 – HDL / 1.1 – 38
The Iranian equation is based on linear regression modeling, which is a good sign, although I would have liked it even better if it was based on nonlinear regression modeling. The reason is that relationships between variables describing health-related phenomena are often nonlinear, leading to biased linear estimations. With a good nonlinear analysis algorithm, a linear relationship will also be captured; that is, the “curve” that describes the relationship will default to a line if the relationship is truly linear (see: warppls.com).
Anyway, an online calculator that implements both equations (Friedewald and Iranian) is linked here; it was the top Google hit on a search for “Iranian equation LDL” at the time of this post’s writing.
As you will see if you try it, the online calculator linked above is useful in showing the difference in calculated LDL cholesterol, using both equations, when fasting triglycerides are very low (e.g., below 50).
The Iranian equation yields high values of LDL cholesterol when triglycerides are high; much higher than those generated by the Friedewald equation. If those are not overestimations (and there is some evidence that, if they are, it is not by much), they describe an alarming metabolic pattern, because high triglycerides are associated with small-dense LDL particles. These particles are the most potentially atherogenic of the LDL particles, in the presence of other factors such as chronic inflammation.
In other words, the Iranian equation gives a clearer idea than the Friedewald equation about the negative health effects of high triglycerides. You need a large number of small-dense LDL particles to carry a high amount of LDL cholesterol.
An even more precise measure of LDL particle configuration is the VAP test; this post has a link to a PDF file with a sample VAP test report.
Reference:
Ahmadi SA, Boroumand MA, Gohari-Moghaddam K, Tajik P, Dibaj SM. (2008). The impact of low serum triglyceride on LDL-cholesterol estimation. Archives of Iranian Medicine, 11(3), 318-21.
Green tea EGCG in low doses boosts fat oxidation by amounts comparable to caffeine

Several studies have reported that green tea improves weight loss, which has largely been attributed to its content of caffeine. A pilot study, however, reports that green tea's main antioxidant catechin, epgallocatechin-3-gallate (EGCG), may also have thermogenic potential.
Thielecke et al of Germany report in the April issue of European Journal of Clinical Nutrition that consumption of EGCG at low doses taken after meals may contribute to increased fat oxidation similarly to caffeine (as much as 35 percent). The same effects of EGCG were not demonstrated while fasting.
The German researchers employed by DSM Nutritional Products performed a randomized, double-blind, placebo-controlled trial on 12 men that were screened for health problems, drugs and smoking. They also excluded men that had taken any dietary supplement within a week of the study.
Each male volunteer consumed an encapsulated supplement over three days (weeklong wash out in between) of either a low dose of EGCG (300mg), high dose of EGCG (600mg), caffeine (200mg), a combination of low-dose EGCG and caffeine (300mg EGCG/200mg caffeine), or a placebo.
The subjects were fed a standard meal of bread, butter, cheese, ham, tomato and cucumber according to the individual energy requiremens of each volunteer, calculated as 5 kcal/kg body weight with 50 percent enrgy from carbohydrates, 35 percent from fats, and 15 percent from proteins. They were prohibited from drinking caffeinated drinks during the study.
Fat and carbohydrate oxidation rates were calculated using a relatively new "respiratory quotient" that measures variance of oxygen consumption (VO2) and carbon dioxide production (VCO2). After three days of each treatment, the researchers took anthropometric measurements for body weight and BMI.
Here are their reported findings:
- 10 of the 12 successfully completed all five supplementation periods
- No adverse effects were reported
- There was no significant difference in fasting blood glucose and insulin from the different supplements
- Energy expenditure was not affected by EGCG
- Caffeine alone and in combination with green tea did have a pronounced effect on fat oxidation
- High dose EGCG boosted fat oxidation by a non-significant 20 percent
- Low dose EGCG surprisingly boosted fat oxidation by 33 percent after meals similarly to caffeine, but not before meals
- Low EGCG (300mg) and caffeine (200mg) maximized fat oxidation, increasing it by 49 percent, after meals
The researchers conclude: "This pilot study provides for the first time evidence that a single green tea catechin, EGCG, can increase fat oxidation in obese men, at least within 2 h after meal intake. Within this postprandial phase, EGCG is equipotent with caffeine with regard to fat oxidation."
My thoughts:
Why did the high dose EGCG not exhibit the same effects as the low EGCG? I understand that there may be a threshold point that is reached by caffeine and EGCG and its influence on fat oxidation, but I have a hard time buying that a low dose of EGCG may be more effective than a high dose. To that end, I'd like to see similar studies appear to clarify the relationship of EGCG on fat oxidation.
However, I am definitely glad to learn that we now know that EGCG does influence fat oxidation and that its effects of potentially improving weight loss have been pinned down to this mechanism instead of others such as reducing fat absorption. I am also glad to confirm that EGCG has no effect on body composition by means of influencing energy expenditure (meaning an influence on how many calories a person burns in a day).
I will continue recommending three or more cups of green tea a day, with or without the caffeine, for helping patients improve their weight loss. Despite the study, however, I think that across the board the most important reason why we continually see patients losing greatest amounts of weight while drinking green tea daily is because they are, at the same time, replacing their sugary beverages such as fountain drinks.
Reference
Thielecke F, Rahn G, Böhnke J, Adams F, Birkenfeld AL, Jordan J, Boschmann J. Epigallocatechin-3-gallate and postprandial fat oxidation in overweight/obese male volunteers: a pilot study. European Journal of Clinical Nutrition advance online publication 7 April 2010; doi:10.1038/ejcn.2010.47.
Thielecke et al of Germany report in the April issue of European Journal of Clinical Nutrition that consumption of EGCG at low doses taken after meals may contribute to increased fat oxidation similarly to caffeine (as much as 35 percent). The same effects of EGCG were not demonstrated while fasting.
The German researchers employed by DSM Nutritional Products performed a randomized, double-blind, placebo-controlled trial on 12 men that were screened for health problems, drugs and smoking. They also excluded men that had taken any dietary supplement within a week of the study.
Each male volunteer consumed an encapsulated supplement over three days (weeklong wash out in between) of either a low dose of EGCG (300mg), high dose of EGCG (600mg), caffeine (200mg), a combination of low-dose EGCG and caffeine (300mg EGCG/200mg caffeine), or a placebo.
The subjects were fed a standard meal of bread, butter, cheese, ham, tomato and cucumber according to the individual energy requiremens of each volunteer, calculated as 5 kcal/kg body weight with 50 percent enrgy from carbohydrates, 35 percent from fats, and 15 percent from proteins. They were prohibited from drinking caffeinated drinks during the study.
Fat and carbohydrate oxidation rates were calculated using a relatively new "respiratory quotient" that measures variance of oxygen consumption (VO2) and carbon dioxide production (VCO2). After three days of each treatment, the researchers took anthropometric measurements for body weight and BMI.
Here are their reported findings:
- 10 of the 12 successfully completed all five supplementation periods
- No adverse effects were reported
- There was no significant difference in fasting blood glucose and insulin from the different supplements
- Energy expenditure was not affected by EGCG
- Caffeine alone and in combination with green tea did have a pronounced effect on fat oxidation
- High dose EGCG boosted fat oxidation by a non-significant 20 percent
- Low dose EGCG surprisingly boosted fat oxidation by 33 percent after meals similarly to caffeine, but not before meals
- Low EGCG (300mg) and caffeine (200mg) maximized fat oxidation, increasing it by 49 percent, after meals
The researchers conclude: "This pilot study provides for the first time evidence that a single green tea catechin, EGCG, can increase fat oxidation in obese men, at least within 2 h after meal intake. Within this postprandial phase, EGCG is equipotent with caffeine with regard to fat oxidation."
My thoughts:
Why did the high dose EGCG not exhibit the same effects as the low EGCG? I understand that there may be a threshold point that is reached by caffeine and EGCG and its influence on fat oxidation, but I have a hard time buying that a low dose of EGCG may be more effective than a high dose. To that end, I'd like to see similar studies appear to clarify the relationship of EGCG on fat oxidation.
However, I am definitely glad to learn that we now know that EGCG does influence fat oxidation and that its effects of potentially improving weight loss have been pinned down to this mechanism instead of others such as reducing fat absorption. I am also glad to confirm that EGCG has no effect on body composition by means of influencing energy expenditure (meaning an influence on how many calories a person burns in a day).
I will continue recommending three or more cups of green tea a day, with or without the caffeine, for helping patients improve their weight loss. Despite the study, however, I think that across the board the most important reason why we continually see patients losing greatest amounts of weight while drinking green tea daily is because they are, at the same time, replacing their sugary beverages such as fountain drinks.
Reference
Thielecke F, Rahn G, Böhnke J, Adams F, Birkenfeld AL, Jordan J, Boschmann J. Epigallocatechin-3-gallate and postprandial fat oxidation in overweight/obese male volunteers: a pilot study. European Journal of Clinical Nutrition advance online publication 7 April 2010; doi:10.1038/ejcn.2010.47.
Labels:
Nutrition News
Saturday, April 10, 2010
Whole milk better for your heart?
Every nutritionist knows (or should know) that a DASH eating plan is incredibly effective for helping patients to lower their blood pressure. A staple on the plan are low-fat or non-fat dairy foods (think 2 percent or skim milk versus whole milk) because they are considered more heart healthy than full-fat dairy, but the results of a 16-year prospective study just published in the European Journal of Clinical Nutritianare suggesting otherwise.
Bonthuis et al are calling for more studies to assess whether or not full-fat dairy may have more cardioprotective benefits than low-fat or nonfat dairy (1). The researchers found that among more than 1,500 adult Australians regularly consuming dairy products, those with highest consumption of full-fat dairy had reduced mortality when compared with those who ate low-fat dairy (1). This was after adjusting for possible confounders such as calcium and vitamin D. Most of the deaths of the participants in the study were related to cardiovascular disease and cancer (1).
The study overall confirms that dairy deserves to continue to be part of DASH and a previously published cohort from Australia that dairy could lower all-cause mortality (2). The study also questions recommendations of avoiding full-fat dairy for long-term protection against chronic disease.
Where did the recommendation to go for the low-fat dairy come from anyway?
The recommendation appeared because of studies that found that low-fat dairy was associated with lower blood pressure, but that full-fat dairy was not. Somewhat recently, the National Heart, Lung, and Blood Institute Family Heart Study in 2006 found an inverse association between prevalent hypertension and consumption of a diet containing dairy low in saturated fat (3).
Given the newest Australian findings, the dairy and blood pressure relationship may be dependent on the fatty acid make-up of the dairy. Could there be something about Australian dairy sources that are cardioprotective? The researchers no doubt must have this data and I imagine less saturated fat and more omega-3s would be involved in their results.
So, don't go switching to whole milk yet. If you like that full-fat flavor, then consider drinking omega-3-fortified dairy.
Just last month in March, a double-blind, cross-over study confirmed that omega-3-fortified dairy foods improved lipid profiles decreasing cardiovascular risk factors (4). The dairy improved omega-3 index, lowered total cholesterol, lowered LDL cholesterol, and lowered triglycerides significantly (4).
Once again, the fact of the matter is that it is the amount of omega-3s in any food that may truly determine how cardioprotective the food really is, as well as its lack of saturated fat and trans fat. Milk is no exception to this nutritional rule.
Reference
1. Bonthuis M, Hughes MC, Ibiebele TI, Green AC, van der Pols JC. Dairy consumption and patterns of mortality of Australian adults. Eur J Clin Nutr. 2010 Apr 7. [Epub ahead of print] Abstract available at http://www.ncbi.nlm.nih.gov/pubmed/20372173.
2. van der Pols JC, Gunnell D, Williams GM, Holly JM, Bain C, Martin RM. Childhood dairy and calcium intake and cardiovascular mortality in adulthood: 65-year follow-up of the Boyd Orr cohort. Heart. 2009 Oct;95(19):1600-6. Epub 2009 Jul 29.
3. Djoussé L, Pankow JS, Hunt SC, Heiss G, Province MA, Kabagambe EK, Ellison RC. Influence of saturated fat and linolenic acid on the association between intake of dairy products and blood pressure. Hypertension. 2006;48:335.
4. Dawczynski C, Marin L, Wagneer A, Jahreis G. n-3 LC-PUFA-enriched dairy products are able to reduce cardiovascular risk factors: A double-blind, cross-over study. Clinical Nutrition. Mar 19. [Epub ahead of print]
Bonthuis et al are calling for more studies to assess whether or not full-fat dairy may have more cardioprotective benefits than low-fat or nonfat dairy (1). The researchers found that among more than 1,500 adult Australians regularly consuming dairy products, those with highest consumption of full-fat dairy had reduced mortality when compared with those who ate low-fat dairy (1). This was after adjusting for possible confounders such as calcium and vitamin D. Most of the deaths of the participants in the study were related to cardiovascular disease and cancer (1).
The study overall confirms that dairy deserves to continue to be part of DASH and a previously published cohort from Australia that dairy could lower all-cause mortality (2). The study also questions recommendations of avoiding full-fat dairy for long-term protection against chronic disease.
Where did the recommendation to go for the low-fat dairy come from anyway?
The recommendation appeared because of studies that found that low-fat dairy was associated with lower blood pressure, but that full-fat dairy was not. Somewhat recently, the National Heart, Lung, and Blood Institute Family Heart Study in 2006 found an inverse association between prevalent hypertension and consumption of a diet containing dairy low in saturated fat (3).
Given the newest Australian findings, the dairy and blood pressure relationship may be dependent on the fatty acid make-up of the dairy. Could there be something about Australian dairy sources that are cardioprotective? The researchers no doubt must have this data and I imagine less saturated fat and more omega-3s would be involved in their results.
So, don't go switching to whole milk yet. If you like that full-fat flavor, then consider drinking omega-3-fortified dairy.
Just last month in March, a double-blind, cross-over study confirmed that omega-3-fortified dairy foods improved lipid profiles decreasing cardiovascular risk factors (4). The dairy improved omega-3 index, lowered total cholesterol, lowered LDL cholesterol, and lowered triglycerides significantly (4).
Once again, the fact of the matter is that it is the amount of omega-3s in any food that may truly determine how cardioprotective the food really is, as well as its lack of saturated fat and trans fat. Milk is no exception to this nutritional rule.
Reference
1. Bonthuis M, Hughes MC, Ibiebele TI, Green AC, van der Pols JC. Dairy consumption and patterns of mortality of Australian adults. Eur J Clin Nutr. 2010 Apr 7. [Epub ahead of print] Abstract available at http://www.ncbi.nlm.nih.gov/pubmed/20372173.
2. van der Pols JC, Gunnell D, Williams GM, Holly JM, Bain C, Martin RM. Childhood dairy and calcium intake and cardiovascular mortality in adulthood: 65-year follow-up of the Boyd Orr cohort. Heart. 2009 Oct;95(19):1600-6. Epub 2009 Jul 29.
3. Djoussé L, Pankow JS, Hunt SC, Heiss G, Province MA, Kabagambe EK, Ellison RC. Influence of saturated fat and linolenic acid on the association between intake of dairy products and blood pressure. Hypertension. 2006;48:335.
4. Dawczynski C, Marin L, Wagneer A, Jahreis G. n-3 LC-PUFA-enriched dairy products are able to reduce cardiovascular risk factors: A double-blind, cross-over study. Clinical Nutrition. Mar 19. [Epub ahead of print]
Labels:
my diet
Friday, April 9, 2010
Getting to the Bottom of Hemorrhoids
When a patient has hemorrhoids (most prevalent in males over 50) then it is always important to evaluate hydration and dietary fiber intake because constipation contributes to risk (1). Sufficient regular water intake and fiber helps to encourage regular bowel movement and alleviate symptoms of constipation.
One can't get to the bottom (excuse the pun) of hemorrhoids, however, without also evaluating the patient's level of activity. A sedentary lifestyle is a major risk factor (spicy foods and alcohol intake are also risk factors) (2). Sitting too long in an office chair, an automobile, in front of the TV, or on a toilet increases pressure on veins in the anus. Exercise promotes circulation and alleviates pressure on the veins, which helps to shrink hemorrhoids and prevent them in the future.
I am also a fan of flavonoids (in particular, micronized purified flavonoids, or Daflon at 500mg) for use with hemorrhoid therapy. There has been at least a few double-blind, placebo-controlled trial that showed flavonoids relieved symptoms associated with hemorrhoids and reduced frequency and severity of hemorrhoid flare-ups (1-4). The evidence behind use of flavonoids, I realize, is limited because of methodological errors and possible bias (5), but in my experience (which I will not explain) they work well.
References
1. Pigot F, Siproudhis L, Allaert FA. Risk factors associated with hemorrhoidal symptoms in specialized consultation. Gastroenterol Clin Biol. 2005 Dec;29(12):1270-4. Available at http://www.em-consulte.com/article/100126.
2. Jiang ZM, Cao JD. The impact of micronized purified flavonoid fraction on the treatment of acute haemorrhoidal episodes. Curr Med Res Opin. 2006 Jun;22(6):1141-7.
3. Danielsson G, Jungbeck C, Peterson K, Norgren L. A randomised controlled trial of micronised purified flavonoid fraction vs placebo in patients with chronic venous disease. Eur J Vasc Endovasc Surg. 2002 Jan;23(1):73-6.
4. Lyseng-Williamson KA, Perry CM. Micronised purified flavonoid fraction: a review of its use in chronic venous insufficiency, venous ulcers and haemorrhoids. Drugs. 2003;63(1):71-100.
5. Struckmann JR. Clinical efficacy of micronized purified flavonoid fraction: an overview. J Vasc Res. 1999;36 Suppl 1:37-41.
6. Alonso-Coello P, Zhou Q, Martinez-Zapata MJ, Mills E, Heels-Ansdell D, Johanson JF, Guyatt G. Meta-analysis of flavonoids for the treatment of haemorrhoids. Br J Surg. 2006 Aug;93(8):909-20.
One can't get to the bottom (excuse the pun) of hemorrhoids, however, without also evaluating the patient's level of activity. A sedentary lifestyle is a major risk factor (spicy foods and alcohol intake are also risk factors) (2). Sitting too long in an office chair, an automobile, in front of the TV, or on a toilet increases pressure on veins in the anus. Exercise promotes circulation and alleviates pressure on the veins, which helps to shrink hemorrhoids and prevent them in the future.
I am also a fan of flavonoids (in particular, micronized purified flavonoids, or Daflon at 500mg) for use with hemorrhoid therapy. There has been at least a few double-blind, placebo-controlled trial that showed flavonoids relieved symptoms associated with hemorrhoids and reduced frequency and severity of hemorrhoid flare-ups (1-4). The evidence behind use of flavonoids, I realize, is limited because of methodological errors and possible bias (5), but in my experience (which I will not explain) they work well.
References
1. Pigot F, Siproudhis L, Allaert FA. Risk factors associated with hemorrhoidal symptoms in specialized consultation. Gastroenterol Clin Biol. 2005 Dec;29(12):1270-4. Available at http://www.em-consulte.com/article/100126.
2. Jiang ZM, Cao JD. The impact of micronized purified flavonoid fraction on the treatment of acute haemorrhoidal episodes. Curr Med Res Opin. 2006 Jun;22(6):1141-7.
3. Danielsson G, Jungbeck C, Peterson K, Norgren L. A randomised controlled trial of micronised purified flavonoid fraction vs placebo in patients with chronic venous disease. Eur J Vasc Endovasc Surg. 2002 Jan;23(1):73-6.
4. Lyseng-Williamson KA, Perry CM. Micronised purified flavonoid fraction: a review of its use in chronic venous insufficiency, venous ulcers and haemorrhoids. Drugs. 2003;63(1):71-100.
5. Struckmann JR. Clinical efficacy of micronized purified flavonoid fraction: an overview. J Vasc Res. 1999;36 Suppl 1:37-41.
6. Alonso-Coello P, Zhou Q, Martinez-Zapata MJ, Mills E, Heels-Ansdell D, Johanson JF, Guyatt G. Meta-analysis of flavonoids for the treatment of haemorrhoids. Br J Surg. 2006 Aug;93(8):909-20.
Labels:
nutr therap
The huge gap between glycemic loads of refined and unrefined carbohydrate-rich foods
I often refer to foods rich in refined carbohydrates in this blog as among the most disease-promoting agents of modern diets. Yet, when one looks at the glycemic indices of foods rich in refined and unrefined carbohydrates, they are not all that different.
The glycemic index of a carbohydrate-rich food reflects how quickly the food is digested and generate a blood glucose response. Technically, it is measured as the area under a two-hour blood glucose response curve following the consumption of a portion of the food with a fixed amount of carbohydrates.
A measure that reflects much better the underlying difference between foods rich in refined and unrefined carbohydrates is the glycemic load, which is the product of the glycemic index of a food by the carbohydrate content in a 100 g portion of the food.
The glycemic load is also the reason for one known fact among diabetics. If a diabetic person eats a very small amount of a high glycemic index food, he or she will have a relatively small increase in blood sugar. If that person consumes a large amount of the same food, the increase in blood sugar will be dramatic.
The table below (click on it to enlarge) shows the remarkable differences between the glycemic loads of foods rich in refined and unrefined carbohydrates. It was taken from an article co-authored by Loren Cordain, Michael R. Eades, and Mary D. Eades (full reference at the end of this post).
At the time of this post’s writing, the article from which the table above was taken had a solid number of citations to it; a total of 74 citations on Google Scholar’s database. It is an excellent article, which I highly recommend reading in full (the link to the online full text is at the end of this post).
What is the reason for the differences in glycemic loads?
The answer is that foods rich in unrefined carbohydrates, even those with a high glycemic index (such as potatoes), are also packed with a number of other things – e.g., micronutrients, fiber, water, and even some protein. An Irish (white) potato is 75 percent water. By comparison, cereal, without milk added, is about 1 percent water. You have to add a lot of whole milk to it to make it a bit healthier. And even unsweetened whole milk is about 5 percent sugar.
There was nothing even remotely similar to modern foods rich in refined carbohydrates in the diet of our Paleolithic ancestors. In fact, the types of food rich in refined carbohydrates shown on the table above are very recent, typically dating back to less than a hundred years ago. That is, they are so recent that it is unlikely that any of us have genetic adaptations to those types of food.
Once one’s glucose metabolism is seriously impaired, which seems to be associated with consumption over many years of refined carbohydrates and sugars (as well as some genetic predisposition, which may have evolved among some of our ancestors), then even the foods with high glycemic index and low glycemic load (e.g., potato) will lead to highly elevated glucose levels if eaten in more than very small amounts.
Insulin resistant individuals should avoid even foods with high glycemic index and low glycemic load, as well as any food that significantly increases their blood glucose levels after a meal, because highly elevated glucose levels are toxic to various tissues in the body. The longer those highly elevated serum glucose levels are maintained, the more damage is done; e.g., 2 hours as opposed to 30 minutes at 180 mg/dl. One reason why they are toxic is because they lead to high levels of protein glycation; this is a process whereby sugar binds to protein and “warps” it, impairing its functions.
Generally speaking, the more glycation is going on in our body, the more accelerated is the aging process.
Reference:
Loren Cordain, Michael R. Eades, Mary D. Eades (2003). Hyperinsulinemic diseases of civilization: More than just Syndrome X. Comparative Biochemistry and Physiology: Part A, 136, 95–112.
The glycemic index of a carbohydrate-rich food reflects how quickly the food is digested and generate a blood glucose response. Technically, it is measured as the area under a two-hour blood glucose response curve following the consumption of a portion of the food with a fixed amount of carbohydrates.
A measure that reflects much better the underlying difference between foods rich in refined and unrefined carbohydrates is the glycemic load, which is the product of the glycemic index of a food by the carbohydrate content in a 100 g portion of the food.
The glycemic load is also the reason for one known fact among diabetics. If a diabetic person eats a very small amount of a high glycemic index food, he or she will have a relatively small increase in blood sugar. If that person consumes a large amount of the same food, the increase in blood sugar will be dramatic.
The table below (click on it to enlarge) shows the remarkable differences between the glycemic loads of foods rich in refined and unrefined carbohydrates. It was taken from an article co-authored by Loren Cordain, Michael R. Eades, and Mary D. Eades (full reference at the end of this post).
At the time of this post’s writing, the article from which the table above was taken had a solid number of citations to it; a total of 74 citations on Google Scholar’s database. It is an excellent article, which I highly recommend reading in full (the link to the online full text is at the end of this post).
What is the reason for the differences in glycemic loads?
The answer is that foods rich in unrefined carbohydrates, even those with a high glycemic index (such as potatoes), are also packed with a number of other things – e.g., micronutrients, fiber, water, and even some protein. An Irish (white) potato is 75 percent water. By comparison, cereal, without milk added, is about 1 percent water. You have to add a lot of whole milk to it to make it a bit healthier. And even unsweetened whole milk is about 5 percent sugar.
There was nothing even remotely similar to modern foods rich in refined carbohydrates in the diet of our Paleolithic ancestors. In fact, the types of food rich in refined carbohydrates shown on the table above are very recent, typically dating back to less than a hundred years ago. That is, they are so recent that it is unlikely that any of us have genetic adaptations to those types of food.
Once one’s glucose metabolism is seriously impaired, which seems to be associated with consumption over many years of refined carbohydrates and sugars (as well as some genetic predisposition, which may have evolved among some of our ancestors), then even the foods with high glycemic index and low glycemic load (e.g., potato) will lead to highly elevated glucose levels if eaten in more than very small amounts.
Insulin resistant individuals should avoid even foods with high glycemic index and low glycemic load, as well as any food that significantly increases their blood glucose levels after a meal, because highly elevated glucose levels are toxic to various tissues in the body. The longer those highly elevated serum glucose levels are maintained, the more damage is done; e.g., 2 hours as opposed to 30 minutes at 180 mg/dl. One reason why they are toxic is because they lead to high levels of protein glycation; this is a process whereby sugar binds to protein and “warps” it, impairing its functions.
Generally speaking, the more glycation is going on in our body, the more accelerated is the aging process.
Reference:
Loren Cordain, Michael R. Eades, Mary D. Eades (2003). Hyperinsulinemic diseases of civilization: More than just Syndrome X. Comparative Biochemistry and Physiology: Part A, 136, 95–112.
Subscribe to:
Comments (Atom)